Für viele Frauen können die Wochen vor der Menstruation oder die Jahre vor den Wechseljahren sich wie ein plötzlicher Identitätswandel anfühlen. Sie reagieren möglicherweise ungewöhnlich heftig, sind erschöpft oder überfordert, als ob ihre Gedanken und Gefühle ihnen nicht mehr gehören würden.
In einer Woche fühlst du dich geerdet und klar; in der nächsten Woche schwindet deine Geduld wegen der kleinsten Kleinigkeit.
Wenn Ihnen das bekannt vorkommt, sind Sie nicht allein und ganz sicher nicht „kaputt“.
Was Sie fühlen, könnten die neurobiologischen Auswirkungen von PMDD (Prämenstruelle Dysphorische Störung) oder der Perimenopause sein , beides Phasen, in denen sich das Gehirn einer umfassenden hormonellen Umstellung unterzieht.
Diese Veränderungen sind keine Anzeichen von Stimmungsschwankungen oder Willensschwäche. Sie sind vielmehr Zeichen dafür, dass sich das Gehirn an neue Rhythmen anpasst – ein komplexer, intelligenter Übergangsprozess.
Dein Gehirn und deine Hormone: Ein Dialog auf Augenhöhe
Hormone beeinflussen nicht nur Ihr Fortpflanzungssystem; sie prägen auch die Art und Weise, wie Ihr Gehirn Emotionen, Konzentration und Energie verarbeitet.
Östrogen wirkt insbesondere wie ein neurochemischer Verstärker und beeinflusst Serotonin, Dopamin und GABA, die alle Stimmung und Kognition regulieren.
Wenn der Östrogenspiegel während der Lutealphase bei PMDS oder während der Perimenopause stark abfällt, können auch diese Neurotransmitter schwanken.
Das Ergebnis? Die Amygdala (das Angst- und Emotionsreaktionszentrum des Gehirns) reagiert stärker, während der präfrontale Cortex (zuständig für Regulation und Entscheidungsfindung) sich vorübergehend beruhigt.
Ihnen könnte Folgendes auffallen:
-
Erhöhte emotionale Sensibilität
-
Gehirnnebel oder Unentschlossenheit
-
Schlafstörungen
-
Reizbarkeit oder Angstzustände, die scheinbar „aus dem Nichts“ kommen
Das Gehirn funktioniert nicht richtig, es passt sich einfach an . Es lernt, in einem sich verändernden Hormonhaushalt zu funktionieren.
„Wir haben gesehen, dass es bei der Heilung des Nervensystems nicht um Kontrolle geht, sondern um Zuhören.“
Die Wissenschaft der emotionalen Volatilität
Bei PMDS und in der Perimenopause wirkt sich die Hormonempfindlichkeit nicht bei jeder Frau gleich aus. Genetische Veranlagung, frühere Stressbelastungen und die Regulation des Nervensystems beeinflussen, wie widerstandsfähig die Gehirnchemie in diesen Phasen ist.
Studien zeigen, dass Frauen mit PMDS häufig empfindlicher auf normale Hormonschwankungen reagieren. Es bedeutet nicht, dass ihre Hormone „schlechter“ sind, sondern dass die Rezeptoren ihres Gehirns stärker auf die Veränderungen reagieren.
Betrachten Sie es so, als ob die Lautstärke Ihres emotionalen Verstärkers erhöht wird – nicht weil Sie schwach sind, sondern weil Ihre neuronalen Verbindungen intensiver reagieren.
Während der Perimenopause beginnt sich die Kommunikation zwischen Eierstöcken und Gehirn zu verändern. Dieser Übergang kann folgende Auswirkungen haben:
-
Serotonin: beeinträchtigt die Stimmungsstabilität und den Schlaf
-
GABA: Beeinflusst Ruhe und Entspannung
-
Dopamin: Motivation und Fokus regulieren
Wenn diese Systeme aus dem Gleichgewicht geraten, kann Ihr Nervensystem alltäglichen Stress als Bedrohung interpretieren und die Kampf-oder-Flucht-Reaktion leichter aktivieren. Deshalb können sich emotionale Überforderung oder Angstzustände verstärkt anfühlen.
Das Gehirn versucht, dich zu schützen
Aus neurowissenschaftlicher Sicht sind die Reaktionen Ihres Gehirns intelligent.
Bei Hormonschwankungen schaltet das Gehirn vorübergehend in einen Schutzmodus, indem es nach Sicherheit sucht, Energie spart und den emotionalen Ausdruck als Überlebensstrategie priorisiert.
Das ist keine Sabotage, sondern Kommunikation.
Ihr Nervensystem könnte Ihnen Folgendes sagen:
„Ich brauche mehr Regulierung.“
„Ich justiere mein Gleichgewicht zwischen Ruhe und Leistung neu.“
„Ich brauche einen ruhigeren Rhythmus und weniger Stressfaktoren, um mich zu stabilisieren.“
Das Erkennen dieses Musters wandelt Selbstverurteilung in Selbstverständnis um.
Ihre Symptome werden zu Signalen – zu aussagekräftigen Daten über die Verbindung zwischen Gehirn und Körper.
Licht, Ton und neuronale Kohärenz
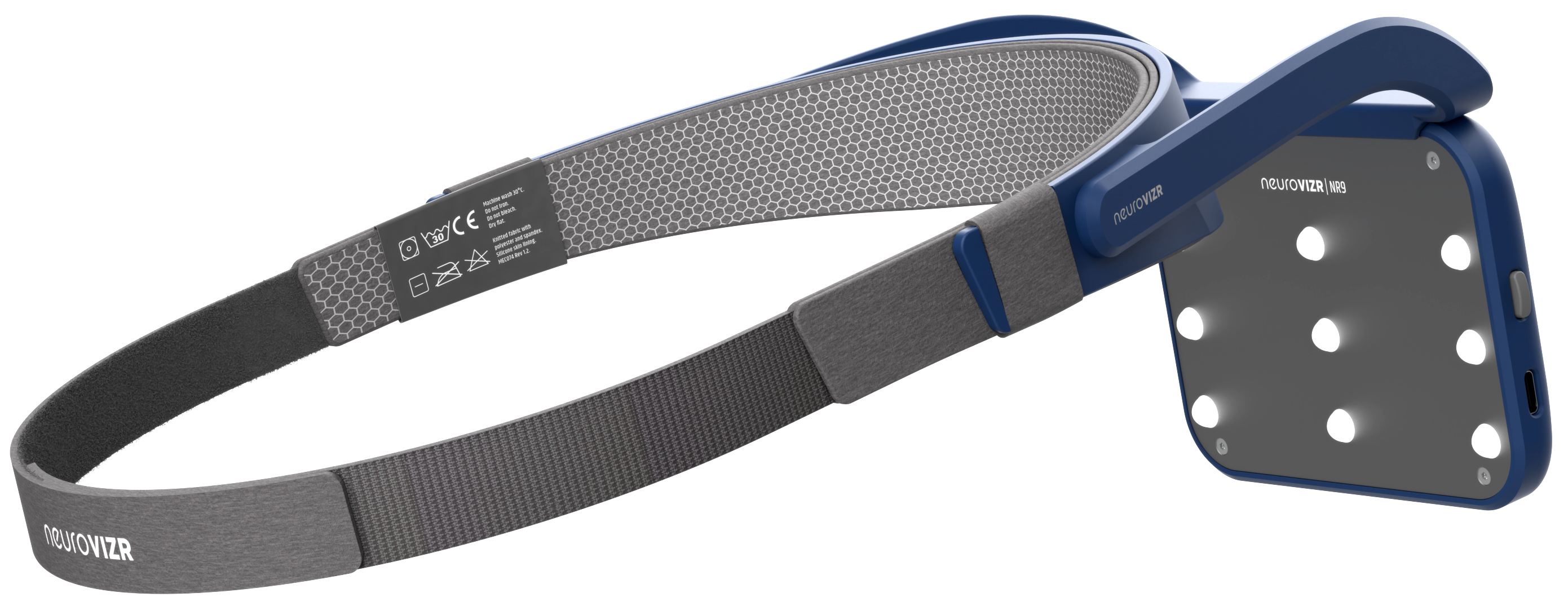
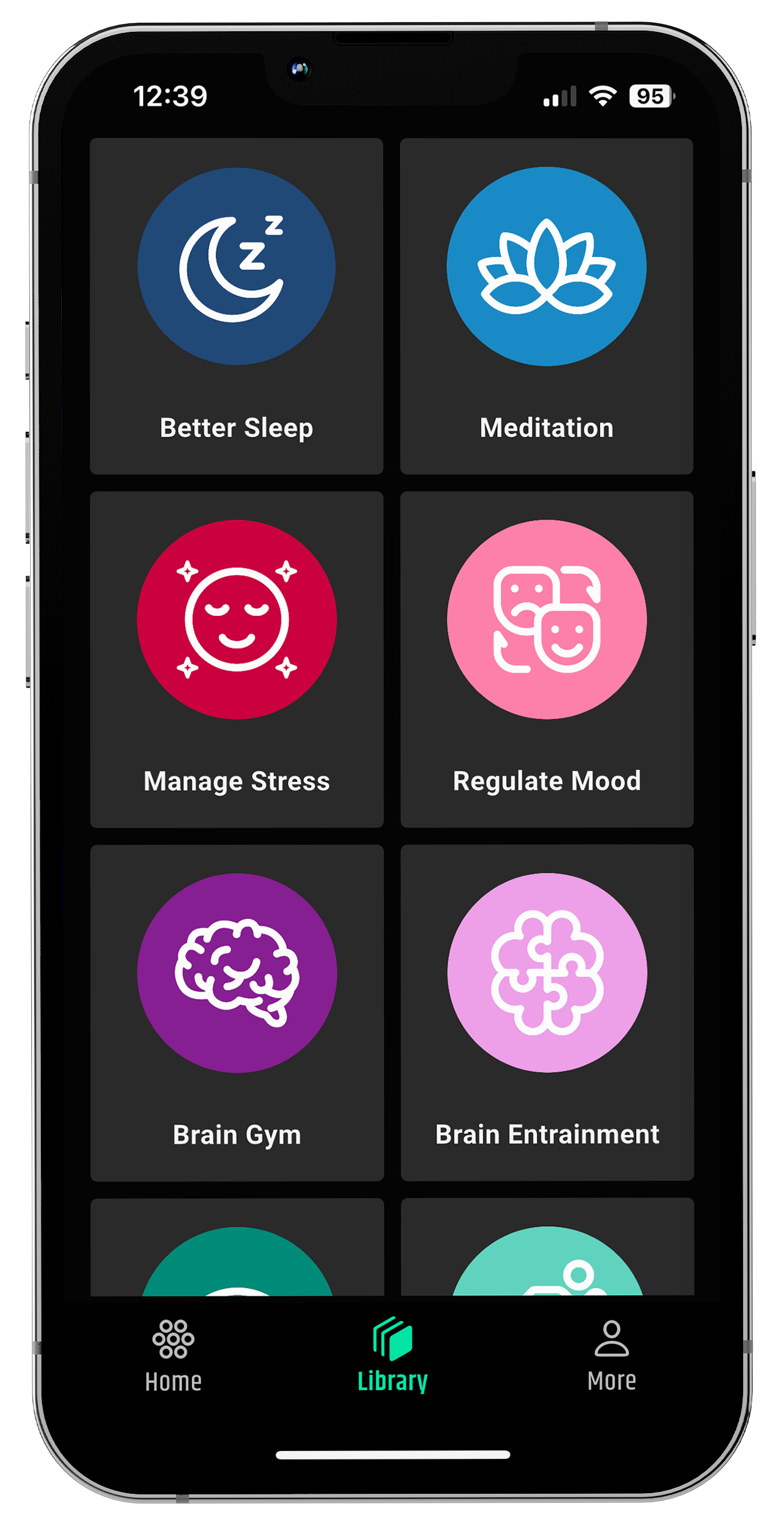
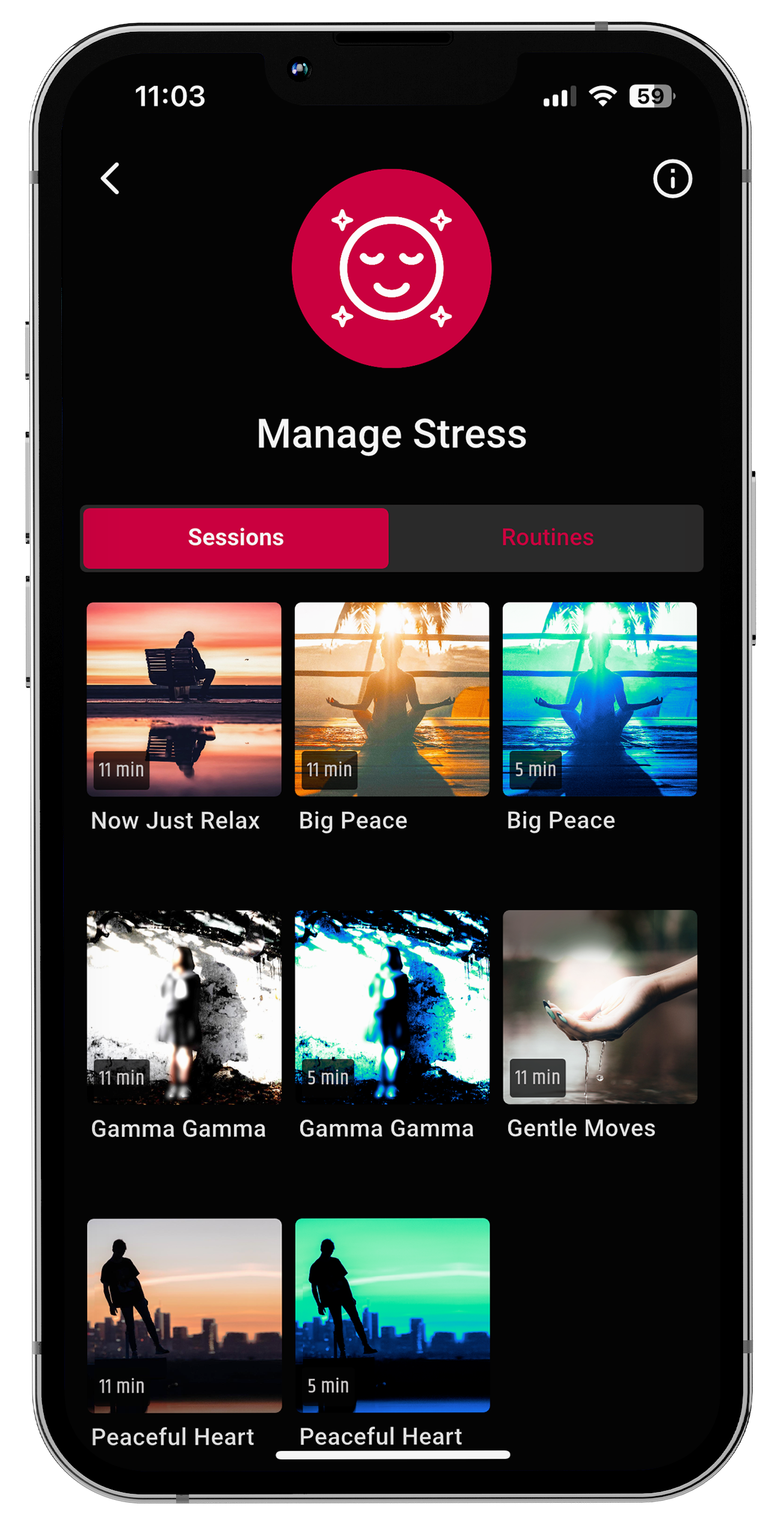
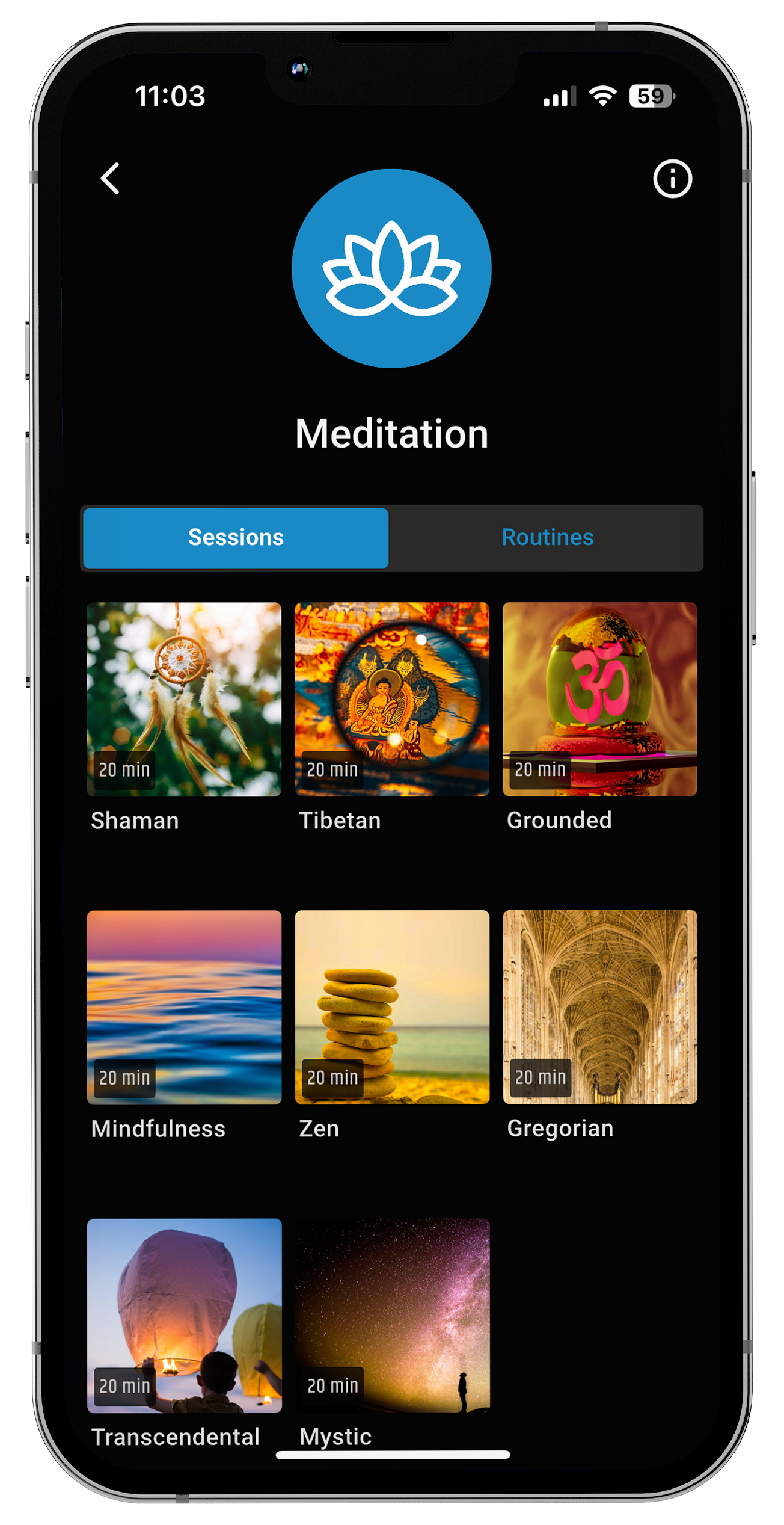
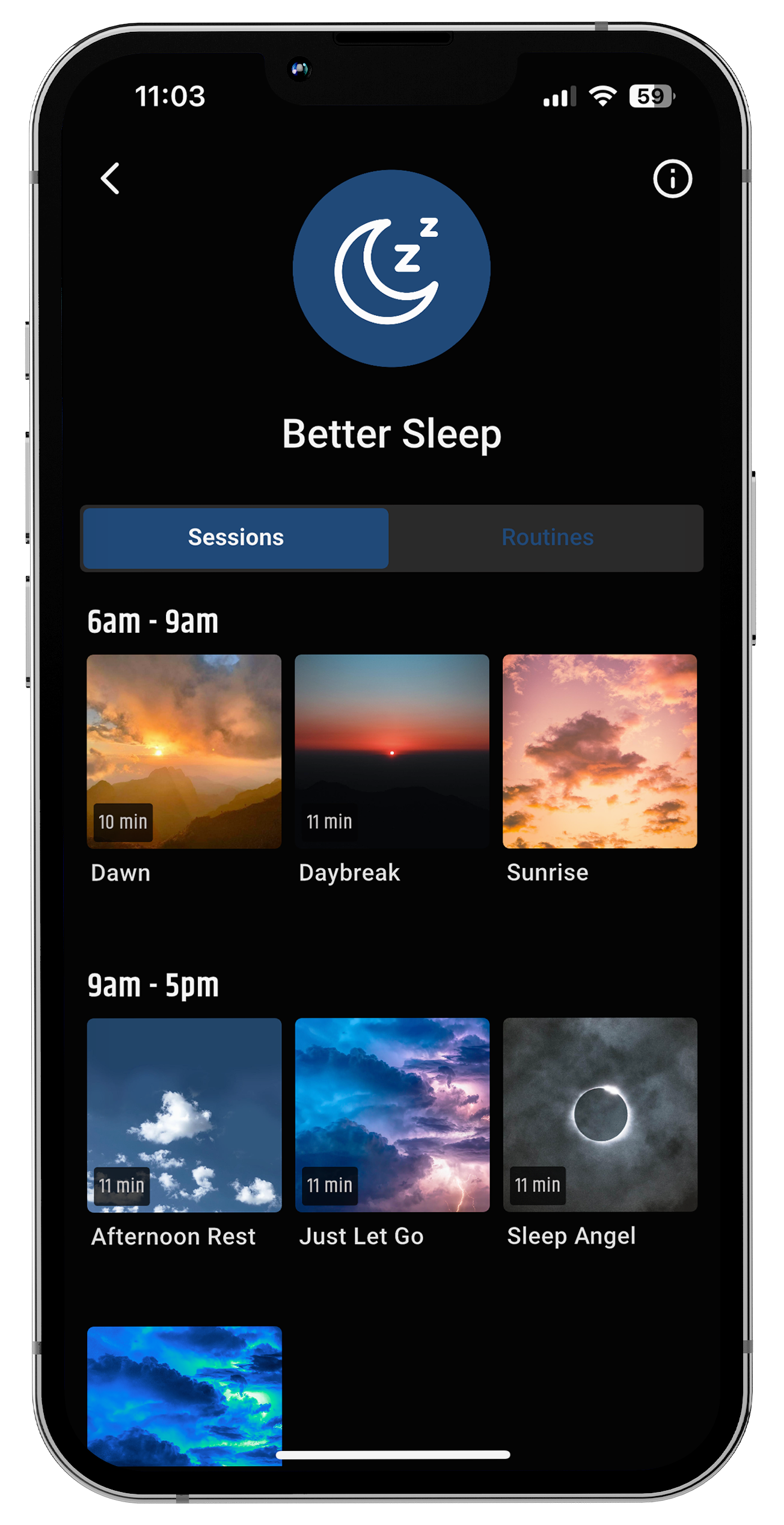
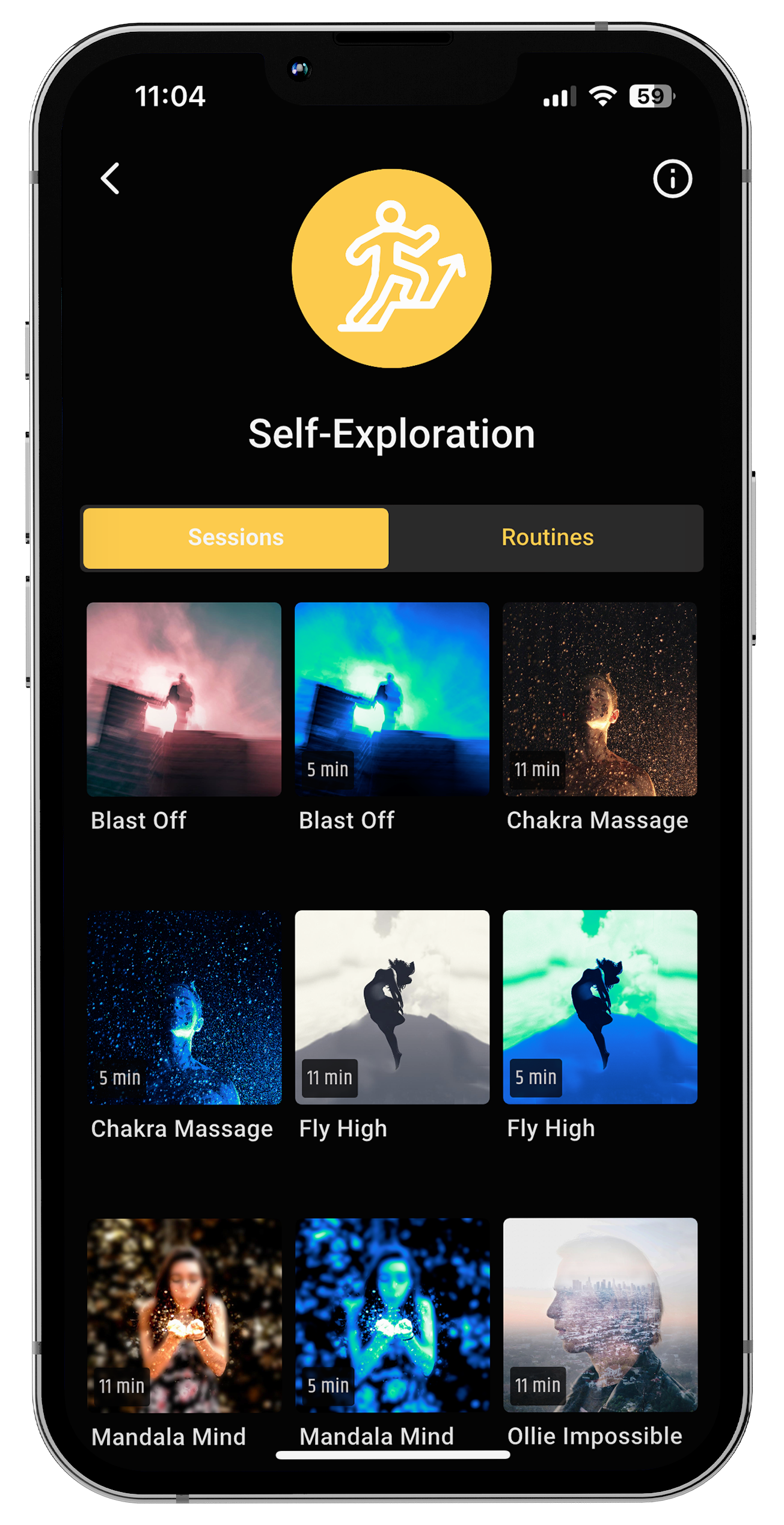
Ein neuer Ansatz zur Unterstützung des Gehirns während hormoneller Umstellungen ist die Neurostimulation mit sanften Licht- und Tonmustern, die die Kohärenz der Gehirnwellen fördern.
Bei neuroVIZR wird dieser Ansatz als visuelle und auditive Neuromodulation bezeichnet . Er nutzt rhythmische, multisensorische Stimulation, um das Gehirn in Richtung Gleichgewicht zu lenken und so die Kommunikation neuronaler Netzwerke zu verbessern.
Während sich herkömmliche Hormon- oder Medikamententherapien auf biochemische Veränderungen konzentrieren, spricht die Neurostimulation direkt den elektrischen Rhythmus des Gehirns an.
Es ersetzt keine medizinische Behandlung, sondern ergänzt sie, indem es die Neuroflexibilität unterstützt – die Fähigkeit des Gehirns, sich an Veränderungen anzupassen und selbst zu regulieren.
Frauen, die diese Art von sensorisch-basiertem Ansatz anwenden, berichten häufig:
-
Sich bei Stimmungsschwankungen ruhiger und ausgeglichener fühlen
-
Verbesserter Schlaf und Konzentration
-
Verringertes Gefühl der Überforderung während hormoneller Zyklen
„Wenn sich Ihre inneren Rhythmen unberechenbar anfühlen, kann ein stetiger äußerer Rhythmus für Ihr Gehirn ein Gefühl innerer Sicherheit wiederherstellen.“
Integration: Zusammenarbeit mit Ihrem Gehirn
Hier sind ein paar schonende Möglichkeiten, Ihr System während der Anpassung zu unterstützen:
-
Körperchecks: Achten Sie auf frühe Anzeichen von Anspannung, Müdigkeit oder Gereiztheit. Behandeln Sie diese als Signale, innezuhalten, nicht weiterzumachen.
-
Rhythmische Regulation: Atemübungen, leichtes Sonnenlicht am Morgen oder achtsame Bewegung helfen, den zirkadianen und hormonellen Rhythmus wiederherzustellen.
-
Somatische Erdung: Warme Kompressen, sanftes Dehnen oder langsames Schaukeln können den Vagusnerv stimulieren und so die emotionale Ruhe fördern.
-
Kognitive Umstrukturierung: Wenn Sie gereizt sind, erinnern Sie sich daran: „Mein Gehirn passt sich an, es funktioniert nicht nicht richtig.“
-
Neurostimulationspraktiken: Die Verwendung von rhythmischem Licht und Ton (wie bei neuroVIZR-Sitzungen) kann dazu beitragen, Ihre neuronalen Rhythmen in Phasen des Ungleichgewichts zu stabilisieren.
Die Neudefinition: Anpassung statt Niedergang
Wenn Frauen verstehen, dass PMDS und die Perimenopause keine Zeichen des Verlustes, sondern der Anpassung sind , ändert sich alles.
Dieses Bewusstsein wandelt Frustration in Neugier, Angst in eine Partnerschaft mit der eigenen Biologie um.
Sie beginnen zu erkennen, dass Ihr Gehirn für Sie arbeitet und Ihre neuronalen Netzwerke neu ausrichtet, um sie an eine neue Lebensphase anzupassen.
Und wenn man dann noch Werkzeuge hinzufügt, die diesen Prozess – Wissenschaft, Selbstmitgefühl und sensorische Kohärenz – sanft unterstützen, schafft man die Voraussetzungen für langfristiges Gleichgewicht und Klarheit.
„Bei der Heilung geht es nicht darum, seine Gefühle zu unterdrücken, sondern darum, zu verstehen, was das Gehirn einem beibringen will.“
Abschluss
PMDS und die Perimenopause sind Einladungen, keine Strafen.
Sie fordern uns auf, langsamer zu werden, zuzuhören und die Intelligenz eines Gehirns im Wandel zu respektieren.
Mit der richtigen Kombination aus neurowissenschaftlichen Erkenntnissen, emotionalem Mitgefühl und praktischen Werkzeugen können Sie diese Phase nicht als Chaos, sondern als Kommunikation erleben.
Bei neuroVIZR übersetzen wir Erkenntnisse der Neurowissenschaften in Sinneserfahrungen, die Ihrem Gehirn helfen, auf natürliche, sichere und schöne Weise wieder in seinen Rhythmus zu finden.
Wichtigste Erkenntnisse
-
Hormonelle Veränderungen bei PMDS und in der Perimenopause beeinflussen die Gehirnchemie und die Emotionsregulation.
-
Diese Veränderungen sind adaptiv; Ihr Gehirn passt sich neuen Hormonmustern an.
-
Neurostimulation durch Licht und Ton kann das neuronale Gleichgewicht und die innere Ruhe fördern.
-
Mitgefühl und Selbstwahrnehmung verwandeln hormonelles Chaos in Kommunikation und Verbundenheit.
Häufig gestellte Fragen
Wird PMDS durch einen zu hohen oder zu niedrigen Östrogenspiegel verursacht?
PMDS wird nicht durch die Östrogenmenge verursacht, sondern durch die Reaktion des Gehirns auf normale Hormonschwankungen. Es handelt sich um eine Überempfindlichkeit gegenüber Östrogen- und Progesteronschwankungen, nicht um dauerhaft hohe oder niedrige Werte.
Kann PMDD von selbst verschwinden?
Die Symptome können sich mit zunehmendem Alter oder durch Änderungen des Lebensstils bessern, aber PMDS verschwindet in der Regel nicht ohne Unterstützung. Stressmanagement, Schlafoptimierung und Hormonbalance sowie der Einsatz neurowissenschaftlich fundierter Regulationsmethoden können die Auswirkungen verringern.
In welchem Alter erreicht PMDS ihren Höhepunkt?
PMDS erreicht seinen Höhepunkt oft im späten 20. bis mittleren 30. Lebensjahr , obwohl manche Frauen auch noch in ihren 40ern darunter leiden , insbesondere wenn sie sich der Perimenopause nähern.
Haftungsausschluss
Diese Inhalte dienen ausschließlich Informations- und Bildungszwecken . Sie sind nicht dazu bestimmt, Krankheiten zu diagnostizieren, zu behandeln, zu heilen oder vorzubeugen . Konsultieren Sie immer einen qualifizierten Arzt oder Therapeuten, bevor Sie Änderungen an Ihrer Gesundheits- oder Wellnessroutine vornehmen. neuroVIZR erhebt keinen Anspruch darauf, PMDS, die Perimenopause oder ähnliche Beschwerden zu behandeln.


















Teilen:
Welttag gegen Stress: Wie Ihnen das Verständnis Ihres Gehirns helfen kann, wieder Ruhe zu finden
Movember – Monat der Männergesundheit 2025