What Is OCD?
Obsessive-Compulsive Disorder (OCD) is a chronic mental health condition involving:
-
Obsessions: intrusive, distressing thoughts (e.g., fear of contamination or harm)
-
Compulsions: repetitive behaviors or mental acts (e.g., excessive washing or checking) that aim to reduce anxiety
OCD affects about 2–3% of the population and is often misunderstood as just being overly clean or organized. In reality, OCD is debilitating and can significantly interfere with daily life.
How Can Trauma Trigger OCD?
Many individuals report that their OCD symptoms began after a traumatic event. While trauma doesn't "cause" OCD in every case, it may:
-
Heighten emotional reactivity
-
Impair coping skills
-
Lead to hypervigilance and fear-based rituals
Common Scenarios Where Trauma Leads to OCD:
-
After a car accident, someone might develop compulsive checking behaviors to ensure safety.
-
Following emotional abuse, a person may develop obsessive fears of being judged or "not good enough."
These behaviors are attempts to regain control after experiencing helplessness.
Can OCD Be Caused by Childhood Trauma?
Absolutely. Childhood trauma is one of the most significant contributors to later development of OCD, especially if it involves:
-
Emotional neglect
-
Physical or sexual abuse
-
Inconsistent caregiving or abandonment
-
Exposure to parental mental illness
Research Insight:
A 2014 study published in Psychiatry Research found that people with OCD reported significantly higher levels of emotional abuse and neglect during childhood compared to control groups.
The brain is especially sensitive during early development. Childhood trauma can alter the amygdala (emotional regulation) and prefrontal cortex (decision making), both of which play roles in OCD.
Trauma-Induced OCD vs PTSD: What’s the Difference?
Competitor content often confuses OCD and PTSD. Here's a clear breakdown:
|
Feature |
Trauma-Linked OCD |
PTSD |
|
Thought patterns |
Intrusive, irrational fears |
Flashbacks or reliving events |
|
Behavior |
Compulsions to “neutralize” fear |
Avoidance, hyperarousal |
|
Focus |
Future fear or imagined harm |
Past trauma and memories |
|
Triggers |
Often vague or illogical |
Directly linked to past event |
In some cases, people can have both conditions especially if the trauma is severe.
OCD and Real-Event Trauma
Sometimes OCD forms around a real event, like a breakup, accident, or mistake. This is known as real-event OCD, where the brain becomes stuck on:
-
“What if I had done things differently?”
-
“Am I a bad person because of what happened?”
-
“Did I cause harm?”
The person may mentally replay the event, seeking certainty or resolution — classic OCD behavior.
Also read - is ocd a disability
Why Trauma Alone Doesn't Always Cause OCD
While trauma is a powerful factor, it typically works in combination with:
-
Genetics: OCD tends to run in families
-
Neurochemistry: Low serotonin and irregular brain circuits
-
Temperament: People who are highly sensitive or perfectionistic may be more vulnerable
In other words, trauma may be the trigger, but not always the root cause.
How to Treat Trauma-Related OCD
1. Cognitive Behavioral Therapy (CBT) with ERP
-
Gold standard for OCD treatment
-
Teaches patients to face fears without performing compulsions
-
Helps retrain thought patterns
2. Trauma-Focused Therapy (EMDR, TF-CBT)
-
Processes the trauma so it no longer drives fear-based behavior
-
Often used when PTSD and OCD overlap
3. Medication
-
SSRIs like fluoxetine and sertraline can reduce OCD and trauma symptoms
-
Medication is usually combined with therapy for better results
4. Mindfulness & Compassion-Focused Therapy
-
Helps people become aware of thoughts without judgment
-
Reduces shame and self-criticism, which are common in trauma survivors
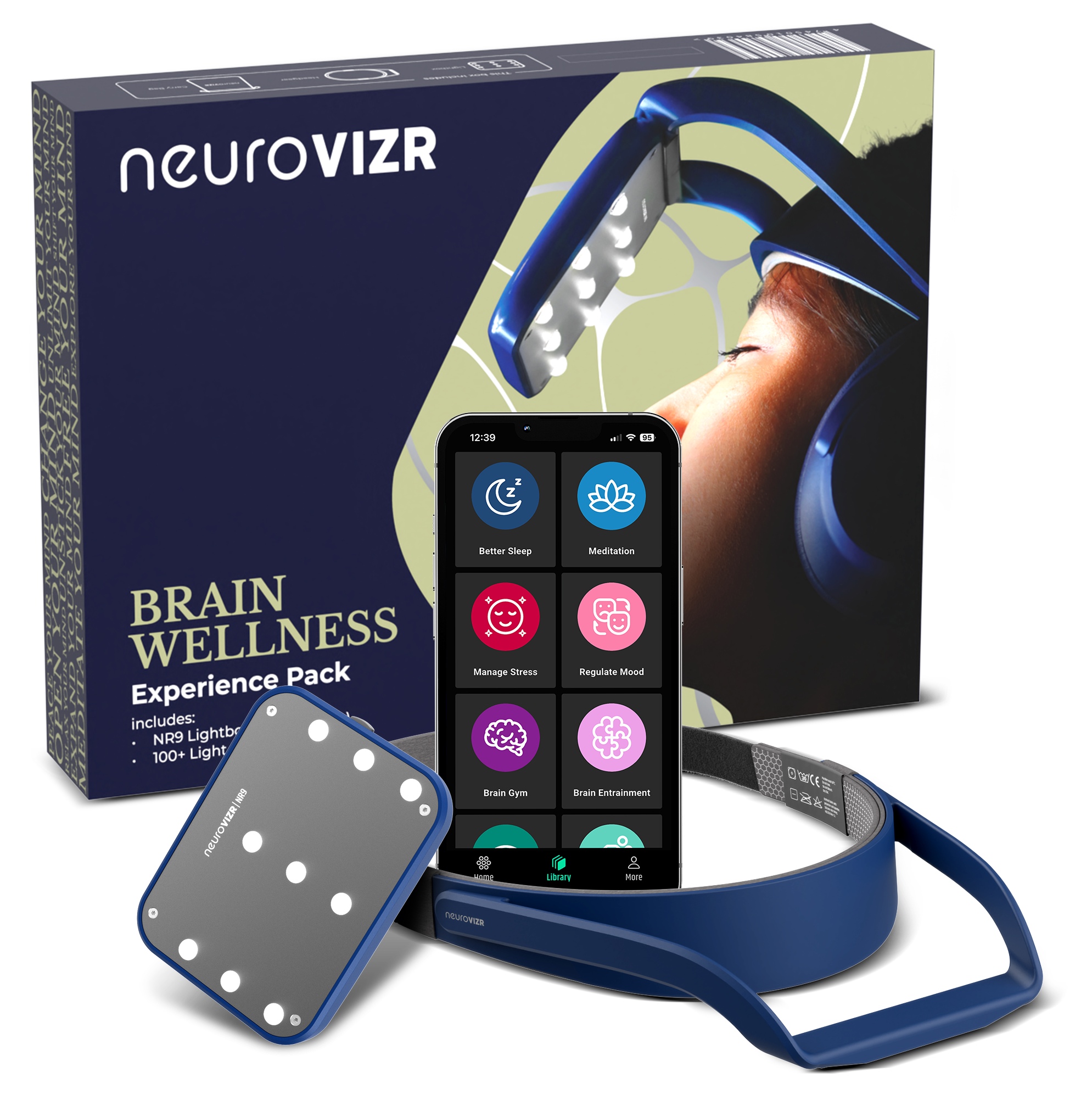
Brain-Based Tech Support: How NeuroVIZR Can Help
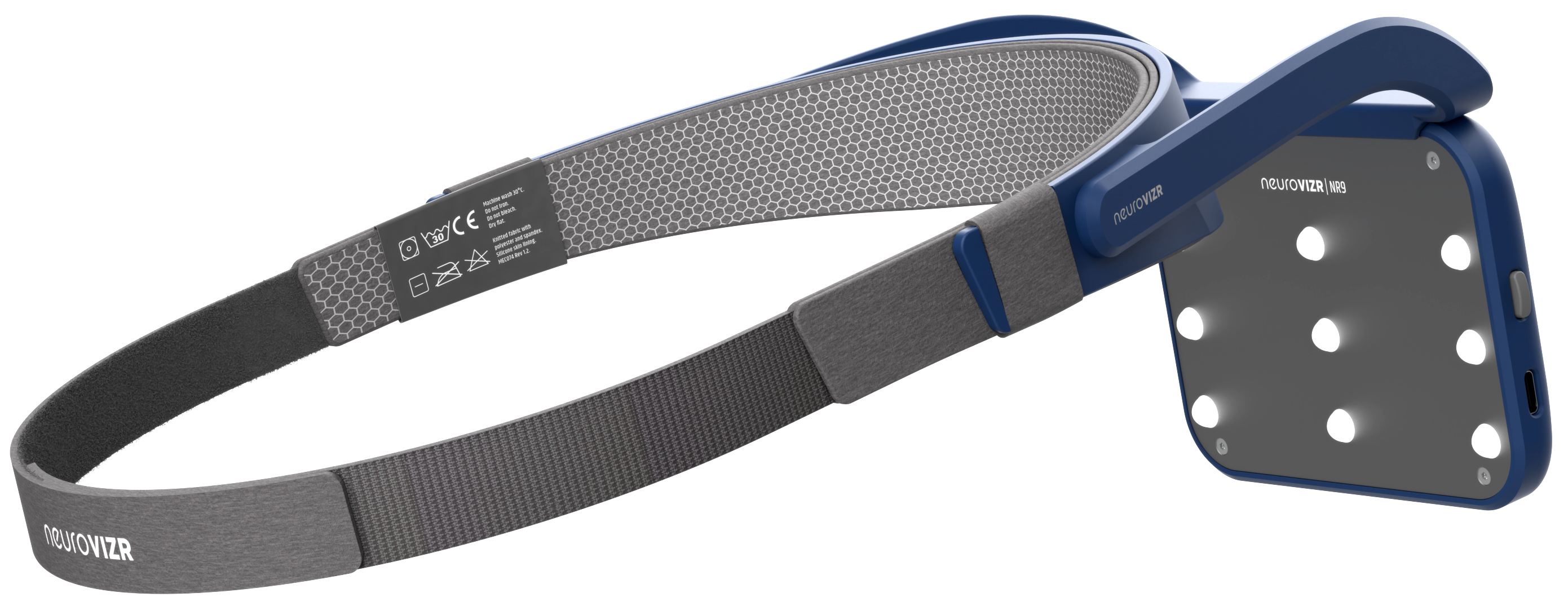
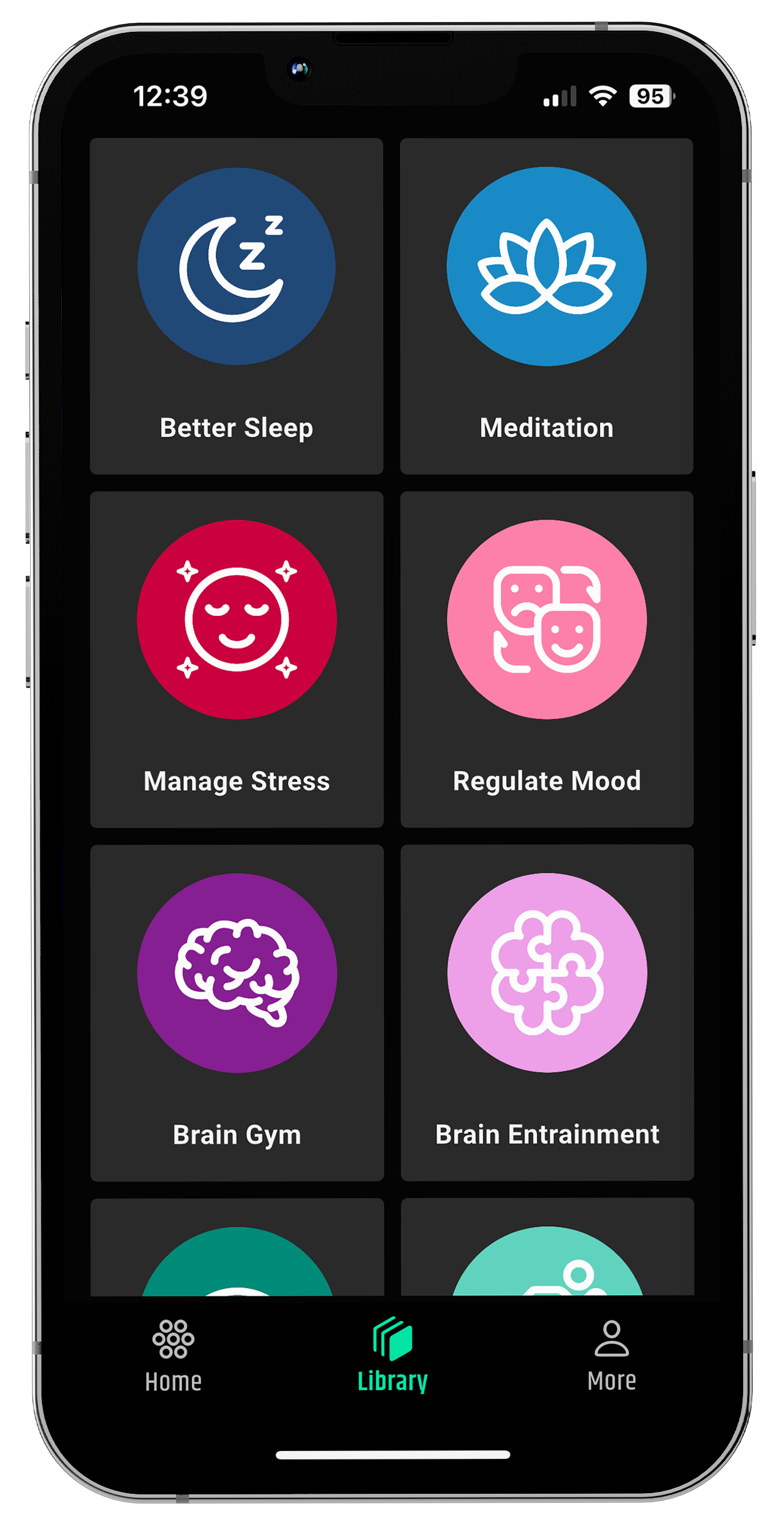
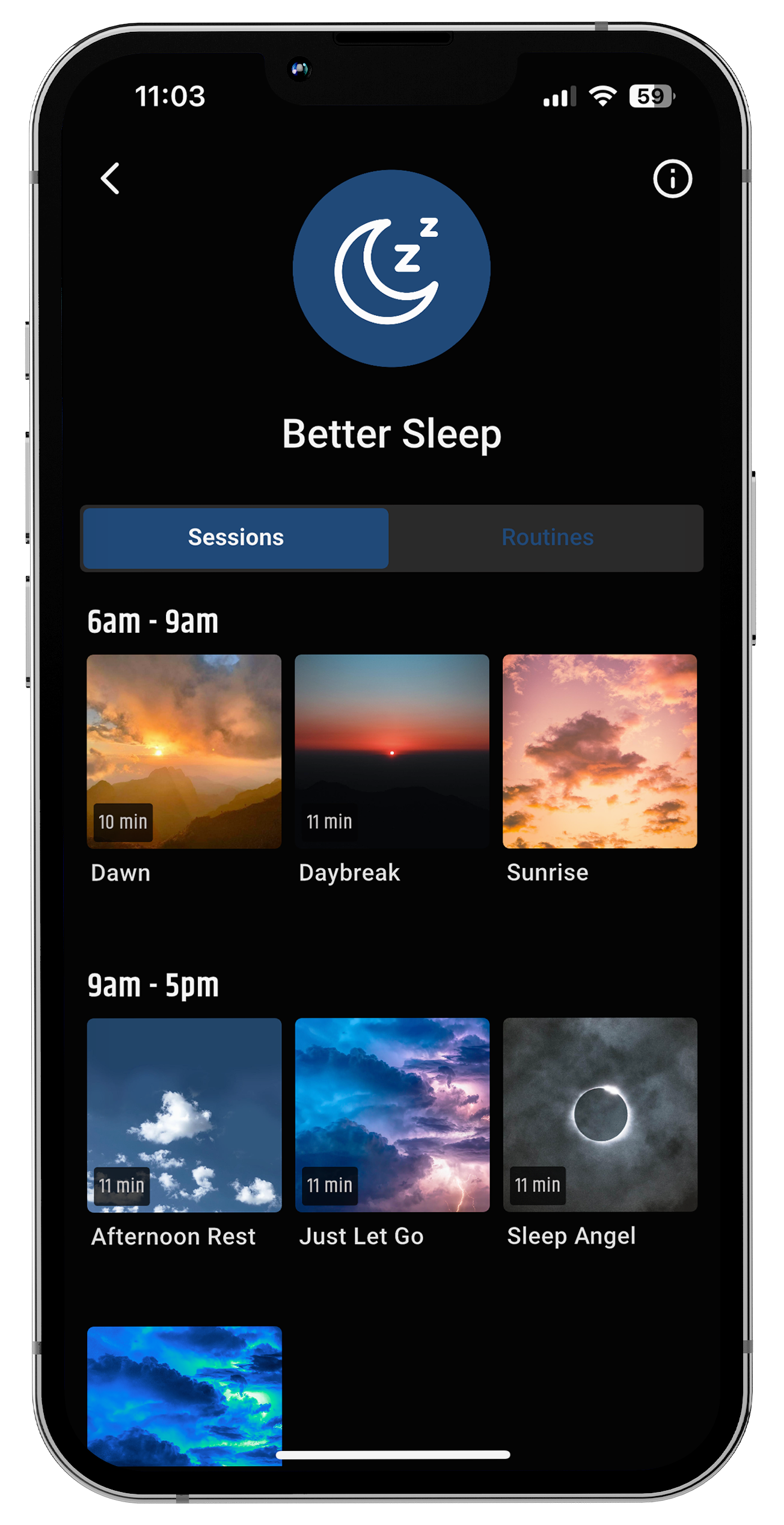
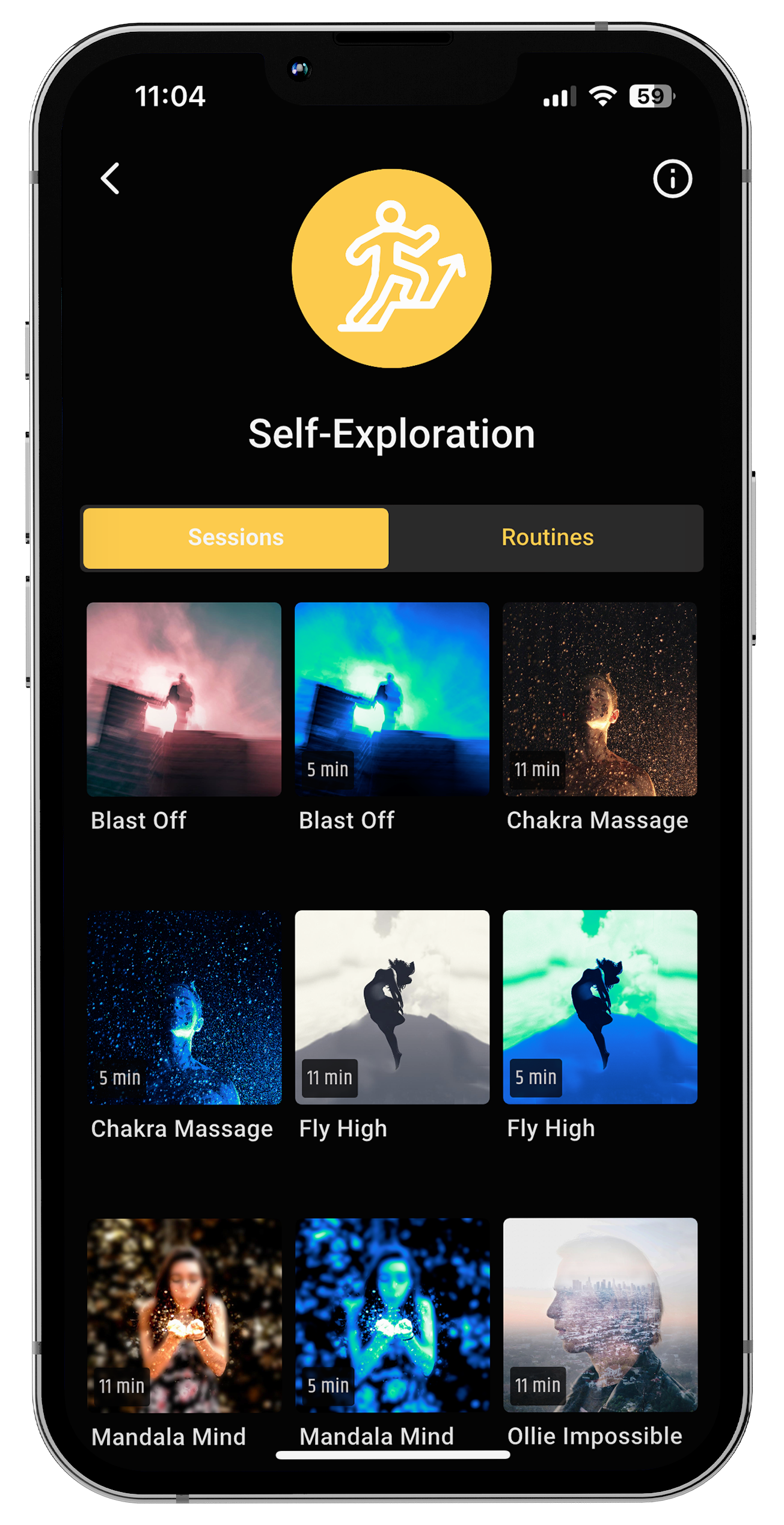
While therapy and medication remain foundational, many individuals are now turning to brain-based wellness tools like the neuroVIZR to support their healing journey.
neuroVIZR brain training app uses light and sound stimulation to gently guide your brain into healthier patterns of activity helping reduce anxiety, obsessive thoughts, and emotional overwhelm that often follow trauma.
Whether you struggle with sleep disruptions, obsessive looping, or emotional shutdown, the neuroVIZR helps regulate your nervous system in a non-invasive, drug-free way.
Why it works for trauma-related OCD:
-
Encourages neuroplasticity (your brain’s ability to rewire and adapt)
-
Calms the amygdala the brain’s fear center
-
Boosts focus, relaxation, and emotional resilience
-
Can be used alongside therapy and medication for a well-rounded recovery plan
Sessions are simple: Just wear the device, choose a guided program (like Calm, Reset, or Sleep), and let your brain respond.
Tips for Managing OCD Caused by Trauma
-
Build a safe routine to regain a sense of control
-
Join a support group (in-person or online)
-
Educate yourself about OCD and trauma
-
Avoid self-blame — neither OCD nor trauma are your fault
-
Practice self-compassion — healing takes time
Final Thoughts: Can OCD Be Caused by Trauma?
Yes trauma, especially childhood trauma, can contribute significantly to the onset or worsening of OCD. However, it's rarely the only cause. OCD is a complex condition shaped by brain chemistry, life experience, and personality.
If you or someone you love is dealing with obsessive-compulsive symptoms tied to trauma, seek professional help. A trauma-informed therapist can make all the difference in recovery.
FAQs
1. What types of trauma cause OCD?
Emotional, physical, or sexual abuse, neglect, accidents, sudden loss, or prolonged stress in childhood or adulthood can all contribute to the onset of OCD.
2. What triggers an OCD episode?
Triggers include stress, trauma reminders, major life changes, illness, sleep deprivation, or even subtle anxiety-inducing situations.
3. Are you born with OCD or is it trauma?
OCD often results from a mix of genetics (you're born with the risk) and environmental factors like trauma, stress, or brain chemistry imbalances.
4. Why is my OCD suddenly so bad?
A sudden spike in OCD may be caused by increased stress, trauma, hormonal changes, lack of sleep, or stopping medication or therapy.
5. Does OCD get worse with age?
OCD can worsen over time without treatment, but with proper therapy and management, symptoms can improve at any age.
6. Can pure OCD be caused by trauma?
Yes, trauma can contribute to Pure OCD (obsessions without visible compulsions), especially when the trauma affects self-worth, fear, or guilt.
Disclaimer: neuroVIZR is a wellness device created to promote relaxation, focus, and overall brain wellness. It is not a medical device, does not provide diagnoses, and is not intended to treat, cure, or prevent any medical condition. The device is not suitable for individuals with epilepsy. Experiences and results may vary from person to person.
















Share:
What Do You Do on Your Hard Days Running? Here’s How to Keep Going When Everything Feels Heavy
How to Stay Focused While Studying?