Many people wonder if obsessive-compulsive disorder (OCD) can arise from a traumatic event. The short answer is yes trauma can sometimes play a role in triggering or shaping OCD symptoms, though the connection is complex and not the only pathway. While not everyone who experiences trauma develops OCD, research shows that stressful or destabilising events can heighten the risk of obsessive thoughts and compulsive behaviours, especially in those who may already be vulnerable.
In this article, we’ll explore what’s known about the relationship between trauma and OCD, how trauma affects the brain, the types of OCD that often emerge after trauma, and what treatment options can offer hope and relief.
What Is the Link Between Trauma and OCD?
OCD is defined by two main features:
-
Obsessions: intrusive, distressing thoughts or fears (e.g., fear of contamination, harm, or loss).
-
Compulsions: repetitive behaviours or rituals aimed at reducing the distress from obsessions (e.g., hand-washing, checking, organising).
Trauma, on the other hand, refers to an experience so overwhelming that it disrupts a person’s sense of safety, stability, or control. Research indicates that trauma can amplify the brain’s threat response system, which may, in turn, fuel the obsessive thought cycles and compulsive behaviours characteristic of OCD.
How Does Trauma Affect the Brain and Behaviour?
Trauma changes the way the brain processes information. Key shifts include:
-
Overactive threat detection: The amygdala becomes hypervigilant, leading to heightened fear responses.
-
Disrupted prediction loops: The brain struggles to accurately filter safe vs. dangerous cues, resulting in constant doubt or “what if” thinking.
-
Need for control: After destabilising events, individuals often seek behaviours that restore a sense of order or predictability.
This biological and psychological ripple effect helps explain why trauma can lay the groundwork for OCD symptoms.
Can Traumatic Events Trigger OCD Symptoms?
Yes. Studies show that traumatic experiences can act as a trigger for OCD onset, particularly in people with a genetic predisposition or co-existing mental health conditions. Importantly, trauma doesn’t have to meet the strict definitions of death, severe injury, or sexual violence (the APA’s official categories).
Even events that are experienced as traumatic such as sudden job loss, unexpected illness, or perceived contamination threats can initiate OCD-like patterns. In these cases, it’s the individual’s subjective experience of destabilisation that matters most.
What Types of OCD Are Common After Trauma?
Research suggests that trauma is more strongly associated with certain subtypes of OCD:
-
Contamination OCD: Following stressful or destabilising events, many individuals develop obsessions around germs, dirt, or infection. Compulsions include excessive hand-washing, cleaning, or sanitising.
-
Hoarding: Around half of individuals with OCD and a trauma history show hoarding tendencies. This behaviour reflects difficulty letting go of items, often linked to fear of future need or loss.
-
Pregnancy-related OCD: Acute onset of OCD has been reported in women during or after pregnancy, often with intrusive thoughts about harm or contamination.
These patterns highlight how trauma can shape the form OCD takes, depending on personal vulnerabilities and life context.
Why Control Becomes Central After Trauma
One of the clearest bridges between trauma and OCD is the need for control. When someone endures a destabilising experience, their world feels unsafe and unpredictable. OCD rituals while distressing in the long run may temporarily restore a sense of control.
For example, a person who experiences a frightening health scare might begin compulsive cleaning or checking behaviours, believing it helps prevent further danger. Unfortunately, these rituals reinforce anxiety, trapping the person in a cycle.
What Research Says About Trauma and OCD
-
60% of OCD patients report onset after a stressful life event.
-
50% of patients with OCD report a history of trauma.
-
Trauma-related OCD is more likely to include contamination fears or hoarding behaviours.
-
Women are at higher risk for pregnancy-related OCD, where trauma and physiological changes may intersect.
While the data is compelling, it’s important to note that not everyone exposed to trauma develops OCD. Genetics, brain chemistry, and resilience factors also play key roles.
Can Treating Trauma Help with OCD?
Yes trauma-focused treatment can support OCD recovery. Since trauma can intensify obsessive fears and compulsions, addressing the underlying event(s) often helps loosen OCD’s grip.
Evidence-based approaches include:
-
Cognitive Behavioral Therapy (CBT), particularly Exposure and Response Prevention (ERP), which helps break compulsive cycles.
-
Trauma-focused therapies, such as EMDR (Eye Movement Desensitisation and Reprocessing) or trauma-informed CBT, which directly target the distressing memories.
-
Medication may also be recommended in some cases, particularly SSRIs, to regulate intrusive thoughts and anxiety.
A combined approach is often most effective, especially when OCD and trauma symptoms overlap.
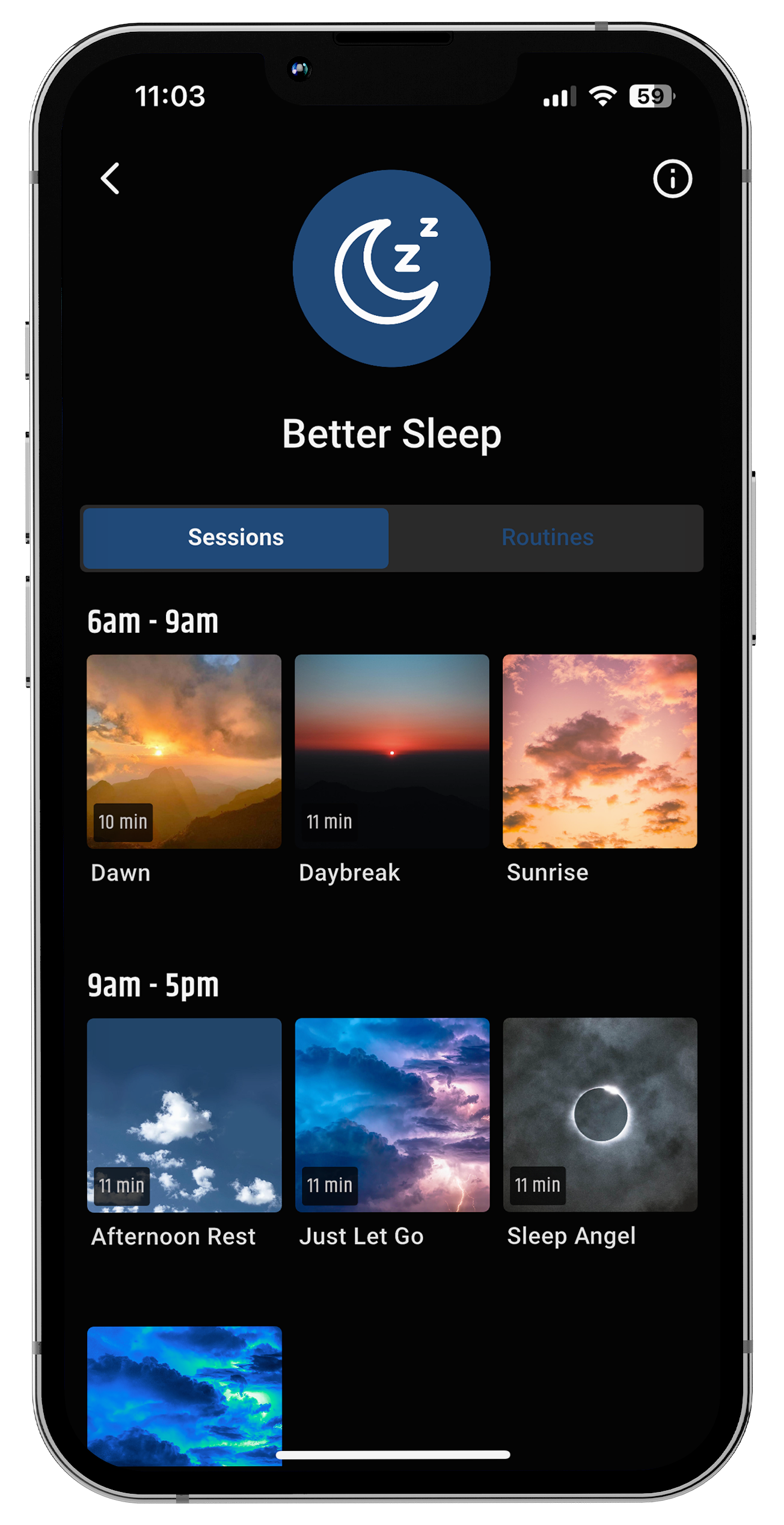
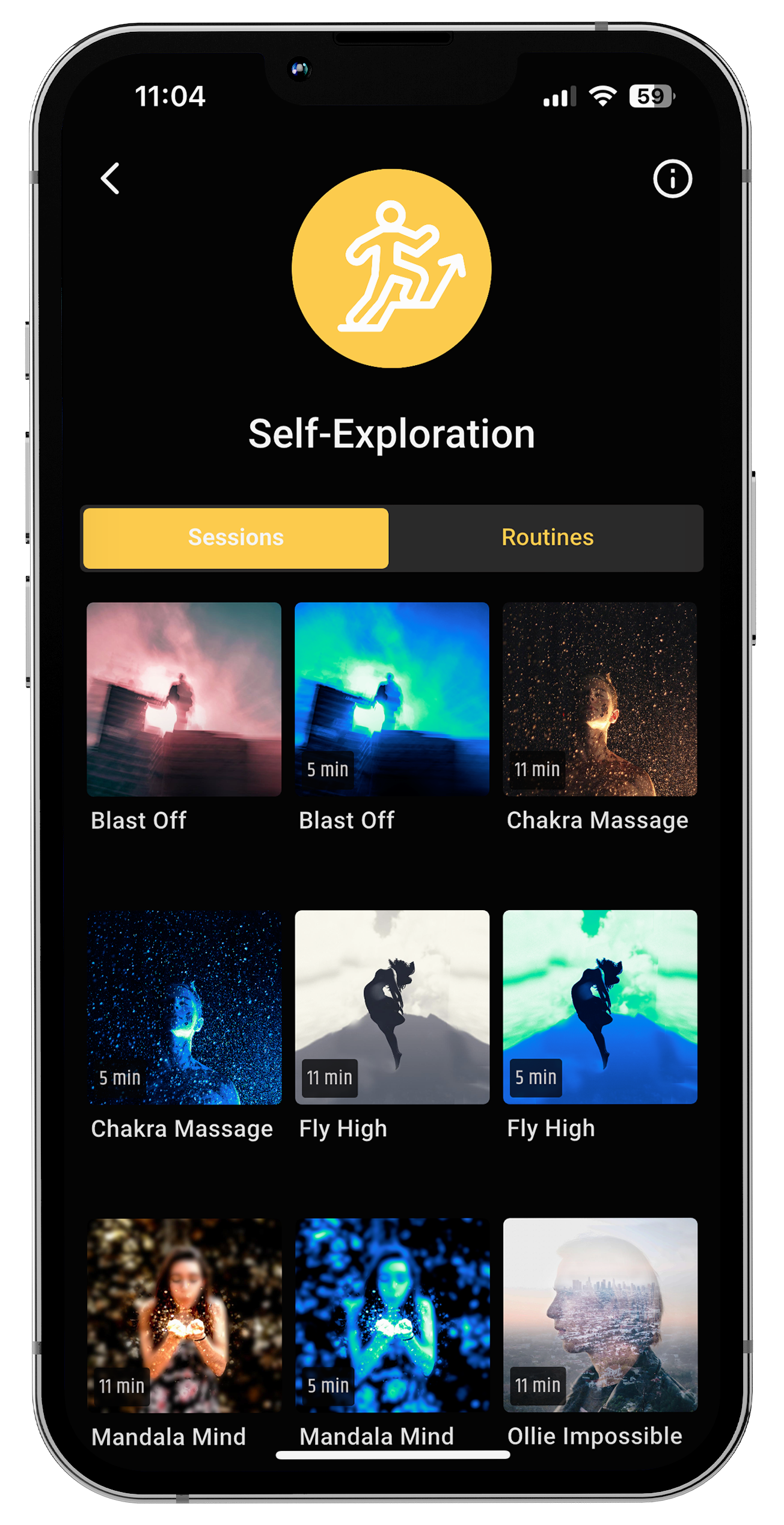
neuroVIZR and Brain Wellness
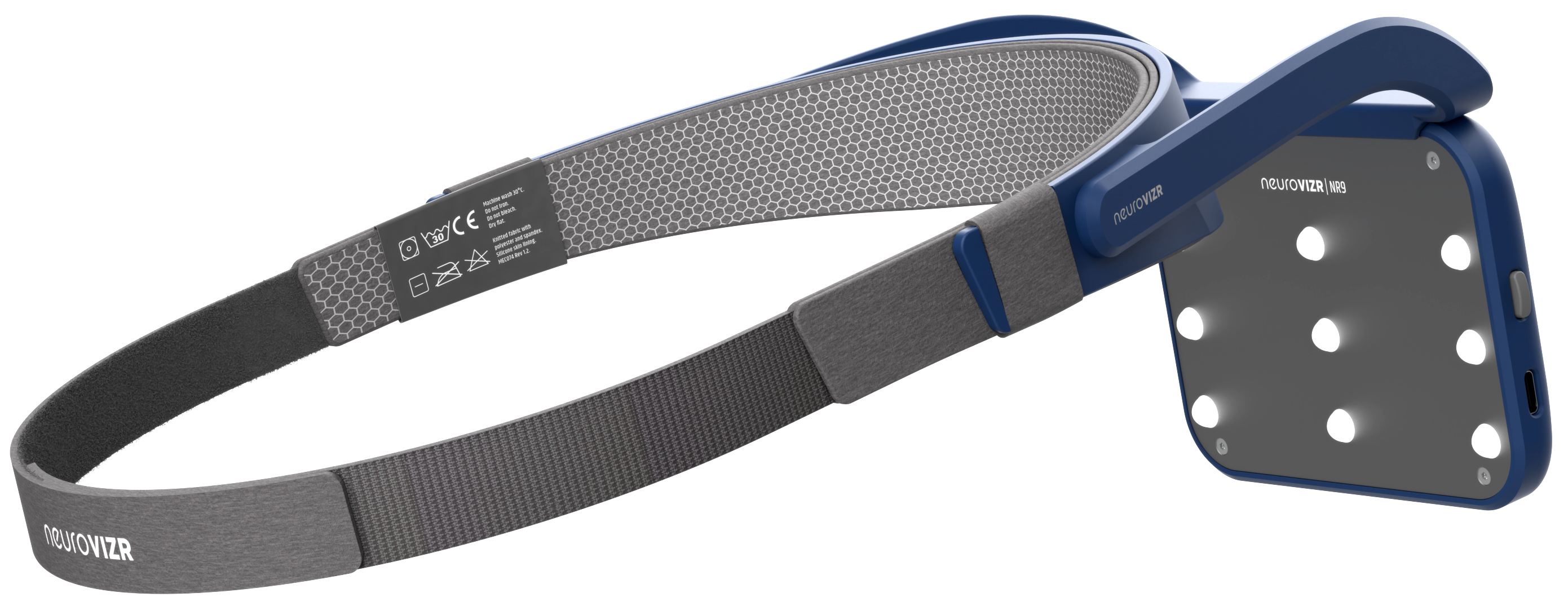
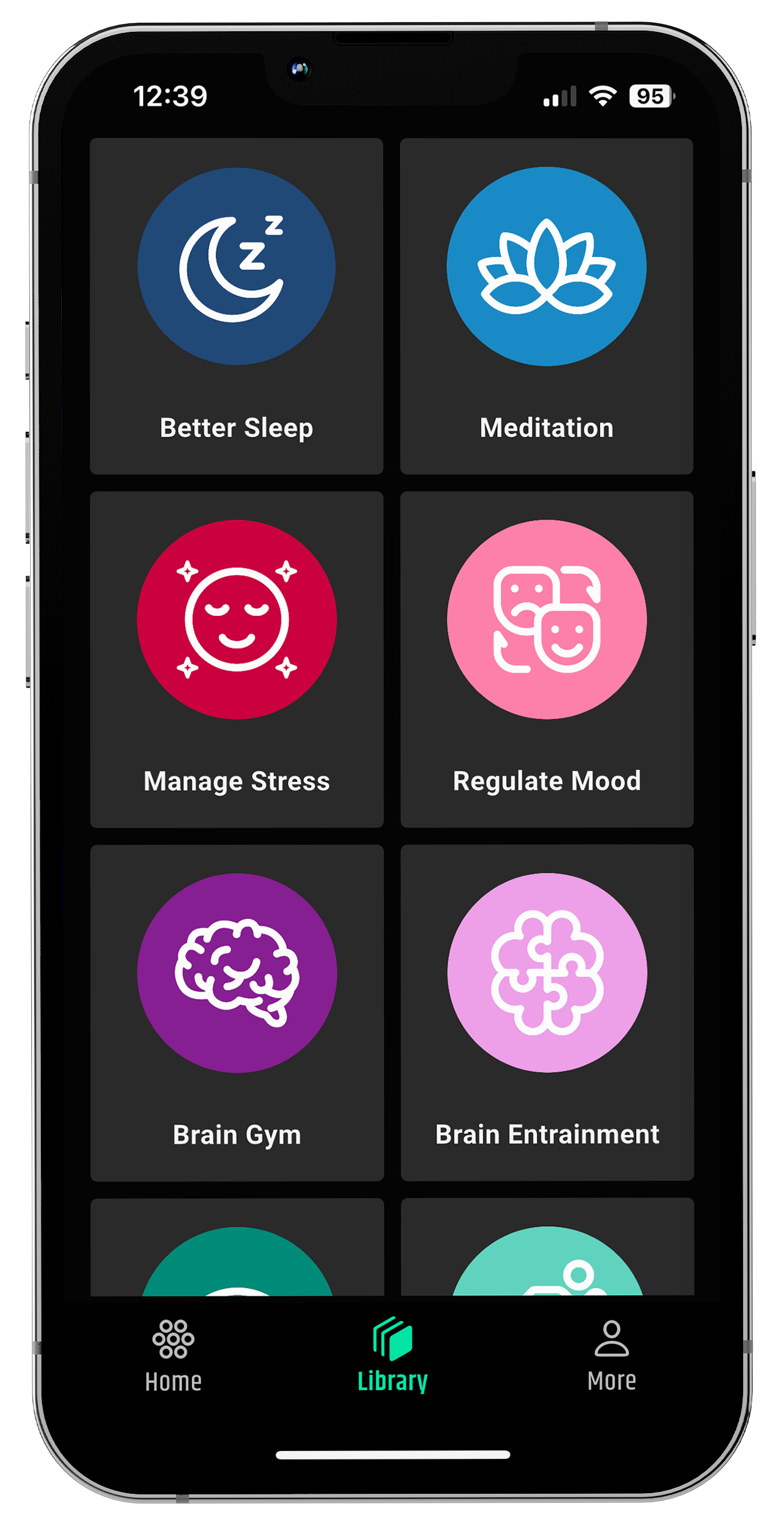
While OCD requires professional mental health care, wellness tools can complement traditional therapy by helping the brain shift out of rigid patterns of stress and hypervigilance. neuroVIZR Brain stimulation headset uses rhythmic light and sound stimulation to encourage brain flexibility, relaxation, and healthier variability.
For individuals recovering from trauma or managing obsessive thought loops, this kind of sensory entrainment can serve as a gentle aid for calming the nervous system, supporting focus, and creating space for new, more adaptive patterns.
Importantly, neuroVIZR is not a medical treatment for OCD but it can be a valuable addition to a broader wellbeing toolkit, helping the brain reset and recharge in everyday life.
When to Seek Support
If you or someone you love is struggling with OCD symptoms especially after a traumatic experience it’s important to seek professional help. Left untreated, OCD can become highly disruptive to daily life, relationships, and overall wellbeing.
Mental health professionals can provide tailored treatment that addresses both trauma history and present-day compulsions. Recovery is possible, and many people experience significant relief with the right support.
Key Takeaway
So, can OCD be caused by trauma? In many cases, yes trauma can act as a trigger or contributing factor for OCD, especially contamination OCD, hoarding, or pregnancy-related subtypes. While not everyone who experiences trauma develops OCD, the overlap is significant enough that mental health professionals now pay close attention to this connection.
Understanding the trauma-OCD link not only helps explain why symptoms appear, but also opens up more compassionate and effective pathways for treatment.
Disclaimer: neuroVIZR is a wellness device created to promote relaxation, focus, and overall brain wellness. It is not a medical device, does not provide diagnoses, and is not intended to treat, cure, or prevent any medical condition. The device is not suitable for individuals with epilepsy. Experiences and results may vary from person to person.

















Share:
INTP and ESTJ Relationship – Understanding Personality Types
What Is Mindless Eating? Causes, Examples, and How to Stop It