You are not alone in feeling a throbbing headache, or even sharp and throbbing pressure in your head just before or during your period. It is a common condition among women to have headaches come as regularly as the menstrual cycle and in some cases so severe that it interferes with work, sleep, or normal existence.
Most of us though are told to simply take a painkiller or just assume that it is normal discomfort and that we just have to put up with it.
But your suffering is not accidental, nor did it mean a weakness in you.
It is a real neurological phenomenon that menstruation can be the cause of headaches and even migraine, and knowing how to transform the experience into frustration to self-pity and knowledgeable mastery.
How Hormonal Changes Cause Headaches?
The hormones and the brain are closely related. During the menstruation period, the estrogen level decreases dramatically and even that single shift may trigger a series of reactions in the brain.
What it does to your brain?
Estrogen affects serotonin, a neurotransmitter, which controls mood and pain.
Pain becomes sensitive when estrogen levels diminish.
Brain blood vessels become hyperirritable and this may cause a pulsating headache.
Inflammation and pain signals can be increased by the release of prostaglandins, chemical substances that are produced during the menstrual process.
In others, this combination can cause menstrual migraine - a severe headache usually one-sided and accompanied by nausea, fatigue, or sensitivity to light and sound.
This is not a stress response or overthinking. It is biology in contact with the nervous system.
How It Feels for Many Women?
-
Menstrual headaches usually come:
-
Some days prior to the period, which is when estrogen levels decrease rapidly.
-
The initial 120 hours of bleeding.
-
Or even after the cycle has come, when the body gets realigned.
Symptoms may show up as:
-
Aching or beating pain at the back of the eyes or temples.
-
Brain fog or difficulty thinking clearly
-
Fatigue or weakness of the face and head.
-
Light or sound sensitivity
-
Nausea or dizziness
Read more - pmdd and perimenopause
Practical Strategies-
It is not about pushing the pain out of your body, but enlightened intelligent use of your physiology.
1. Stay ahead of the pain
When you can tell when your headaches will happen, then help your brain out in advance - hydration, regular sleep and healthy eating can help.
2. Practice calming methods of the nervous system.
Soft movement, breathwork and sensory calming help lower levels of pain by allowing the brain to move off of threat response into regulation.
3. Lessen the effects of inflammation.
The spikes of caffeine, lack of sleep, dehydration, and missing meals may make the signals of pain more prominent in hormonal fluctuations.
4. Track patterns
The trick is to know when your headaches occur, rather than being surprised.
5. Consult a doctor when necessary.
In case headaches are very severe, or disabling, menstrual migraine support plans have been found to be helpful.
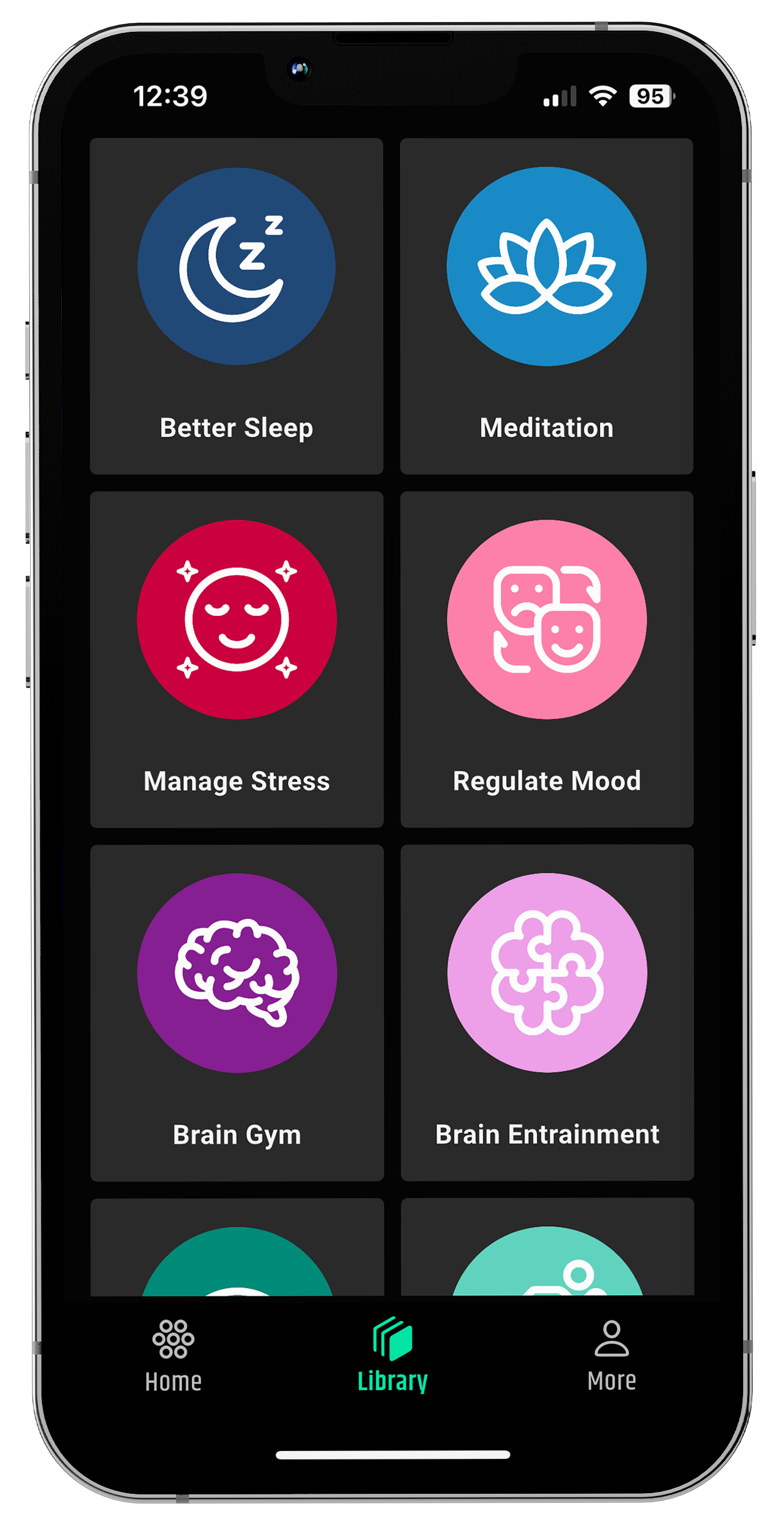
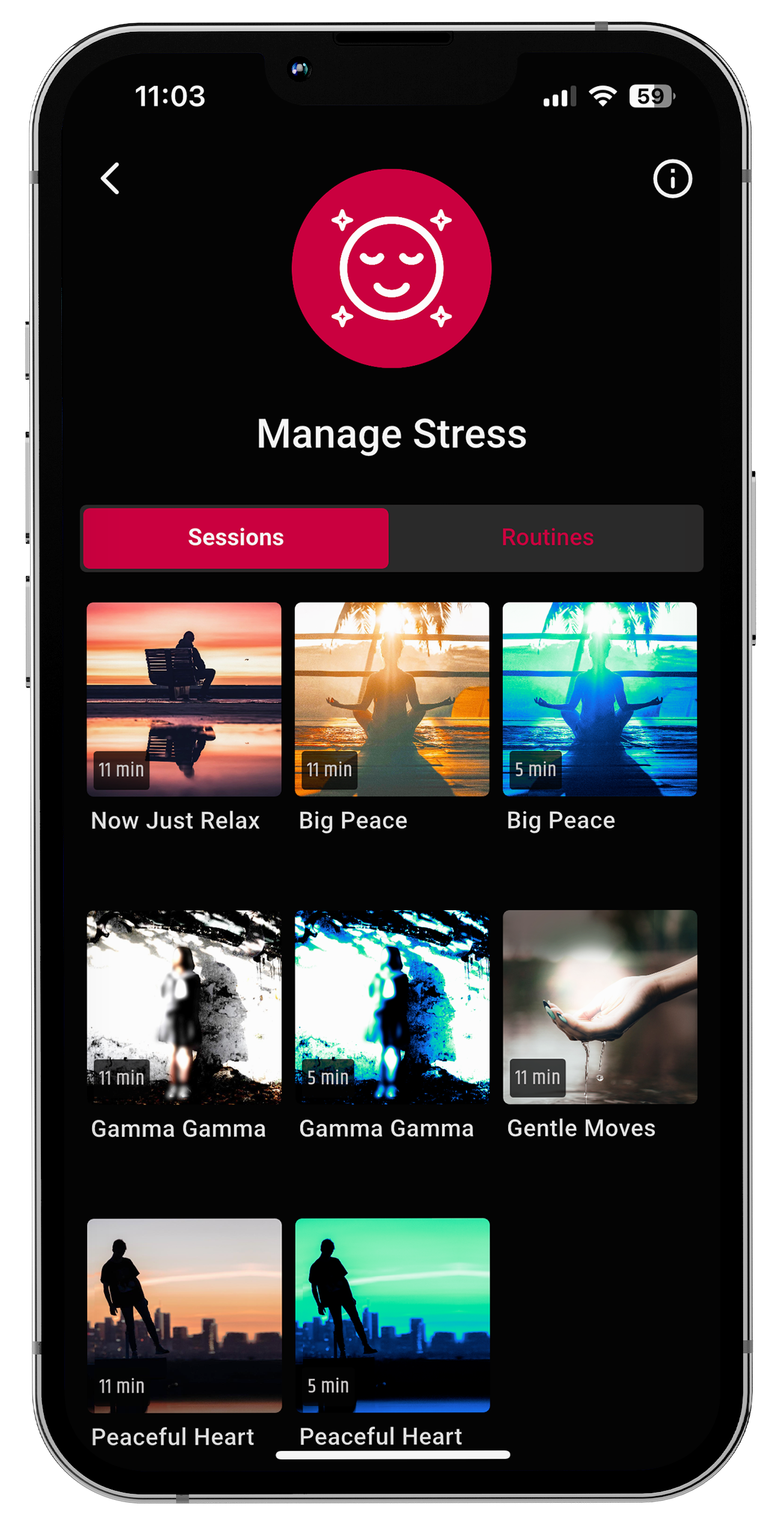
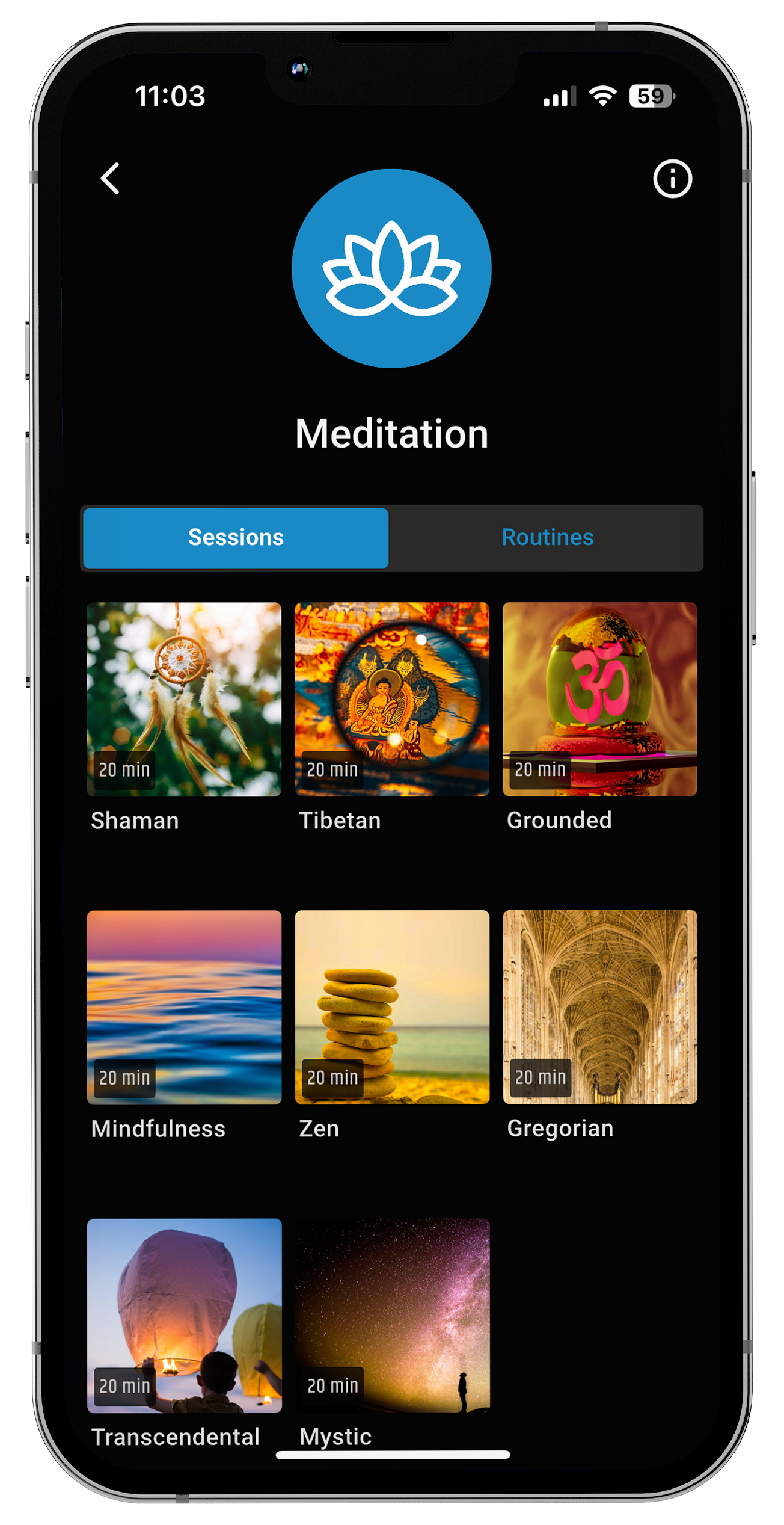
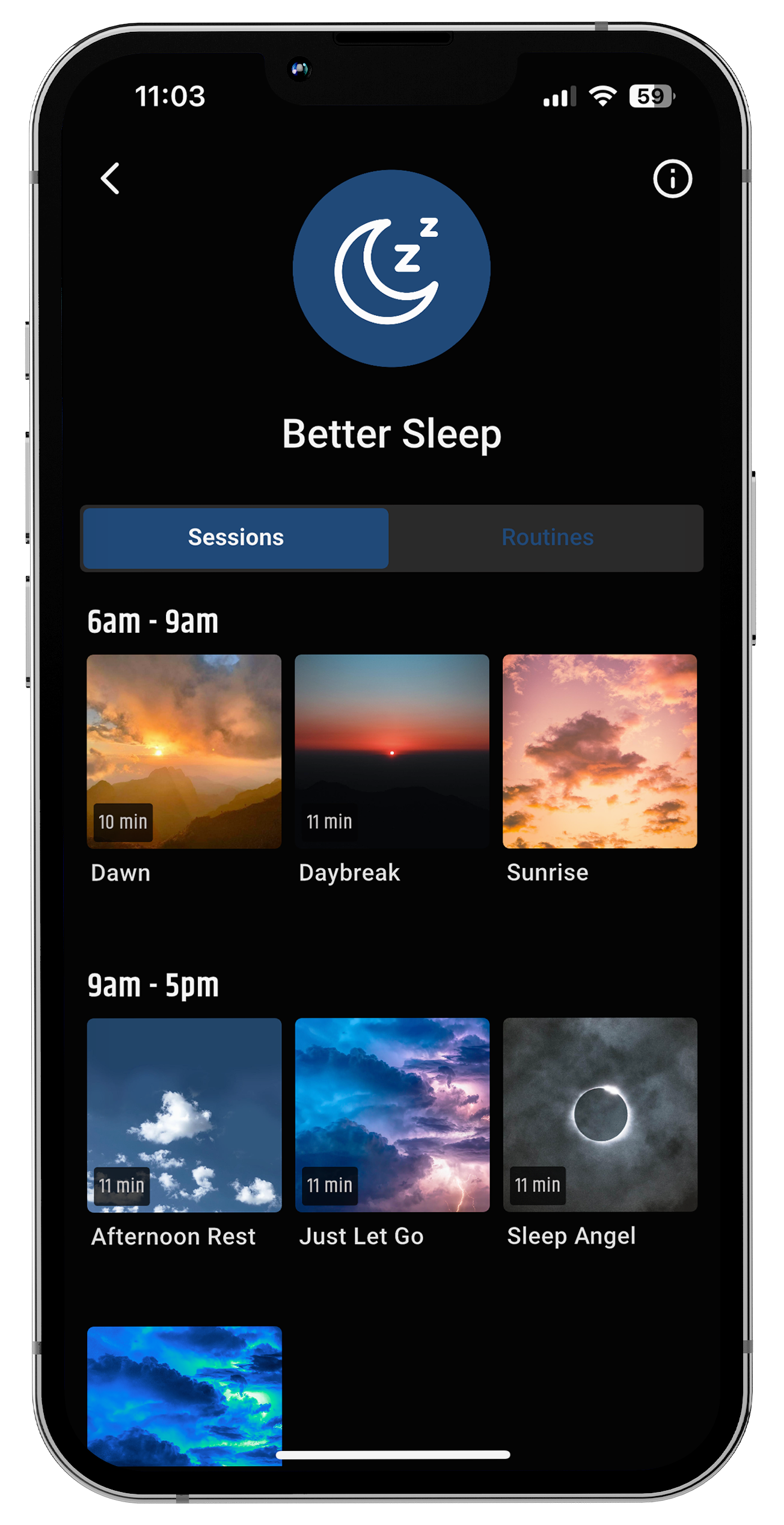
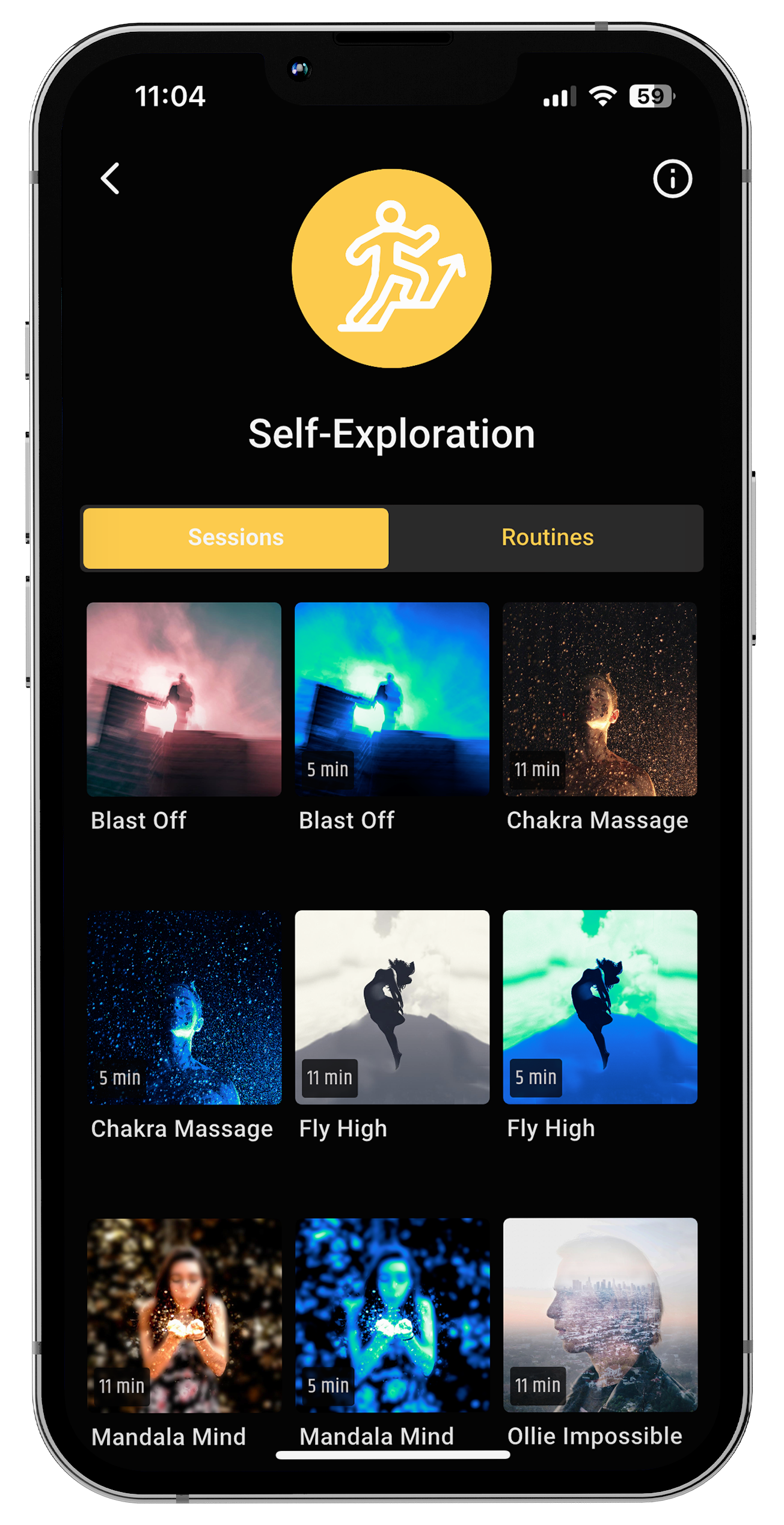
How neuroVIZR Supports?
neuroVIZR provides light and sound programs that are used to allow the user to experience various brain-state experiences, e.g. relaxation, focus, calm, etc. Sensory tools can be used to provide a more supportive environment or be used to aid mental clarity during periods when the body and mind are more sensitive or overwhelmed such as around the time of menstruation. Although each of the experiences is unique, and outcomes differ, the application of neuroVIZR can be included in a personal routine of slowing down, reconnecting with the body, and finding a moment of relaxation when it is needed.
Key Takeaways
-
Yes, menstruation can cause headaches due to hormonal shifts affecting brain chemistry.
-
The sudden drop in estrogen increases pain sensitivity and migraine risk.
-
Inflammation, stress, sleep changes, and prostaglandins can intensify symptoms.
-
With awareness and nervous-system support, headaches can become more manageable.
-
Understanding the science helps transform frustration into informed self-care.
Conclusion
Menstrual headaches are a real neurological response to hormonal changes, not something to “push through.” When estrogen drops, the brain becomes more sensitive to pain, which is why headaches around your period are common and valid. Understanding what’s happening inside your body helps shift the experience from frustration to compassion and empowers you to support your nervous system more gently. Your body isn’t failing you, it's adapting, and you’re doing your best.
FAQs
1. What do period headaches feel like?
Period headaches feel like a throbbing or heavy pain on one side or both sides of the head. Many women also feel pressure behind the eyes, nausea, and sensitivity to light or sound.
2. What are the top 3 causes of headaches?
-
Hormonal changes (estrogen drop before periods)
-
Stress & poor sleep
-
Dehydration and irregular eating habits
3. How do you get rid of menstrual headaches?
Drink plenty of water, rest properly, use a cold compress on the head, take magnesium-rich foods, and use pain relievers like ibuprofen if needed (doctor advice recommended).
4. How long do menstruation headaches last?
Menstrual headaches usually last from a few hours to 2–3 days, depending on hormone levels and stress.
Disclaimer
The content provided in this article is for educational and informational purposes only. It is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of a qualified healthcare provider with any questions you may have regarding a medical condition or before making decisions about your health.
Content References
-
American Migraine Foundation
-
National Headache Foundation
-
Cleveland Clinic
-
Mayo Clinic Women’s Health
-
Johns Hopkins Medicine
-
Harvard Medical School Health Publishing
-
World Health Organization Women’s Health
-
The Migraine Trust


















Share:
Hyperactivity Disorder in Adults Symptoms
Perimenopause Anxiety Disorder: Causes, Symptoms, Diagnosis & Treatment