In case your migraines appear to accompany your menstrual cycle, then you are not dreaming. To most individuals, the days leading up to, or during menstruation cause a type of headache, more severe, more intense and more sensory and thus becomes more difficult to treat. It’s not just pain. It is light, but sharper, sounds louder, and the nervous system that apparently it loses its customary forbearance.
Menstrual migraines are not an individual failure and the body is over reacting. They are an unsurprising brain-body state, one that should not be opposed but rather understood.
Read more - perimenopause anxiety disorder
What Is Really Going on in the Brain?
The majority of explanations end on hormones, and in particular estrogen. And even though hormonal changes are the tale, they are not the entirety.
The brain is more excitable as the level of estrogen decreases before the menstruation period. This influences the processing of the information of sensory nature, especially those pathways associated with perception and pain.
Key changes include:
-
Hypersensitivity in the trigeminal nerve, which is an important pathway in the processing of pain in migraine.
-
Less sensory filtering that is, light, sound, smell is less dampened by the brain.
-
The instability of the nervous system when the balance between the inhibitory and the stimulating signals is weakened.
To put it simply: at this stage, your brain is more difficult to quiet the incoming stimuli.
This explains the reason why menstrual migraine is usually accompanied by a high level of sensitivity to light, intolerance to sound, nausea or withdrawal. The brain is not weak, it is momentarily functioning on a high level.
Why These Migraines Are Different (and Worse)
It is observed by many individuals that menstrual migraines are more stubborn to the general strategies. The reason is that they are not only precipitated by a circumstance outside themselves such as stress or sleep deprivation but they are a result of an internal process of a brain chemical and rhythm change.
This will make one feel powerless:
“Why does this keep happening?”
Why not be able to stop it when it begins?
The only thing that is lacking in the talk is reassurance:
This has nothing to do with willpower and bad coping. It is one of those brains that require different conditions within this window.
Working With a Sensitive Brain, Not Against It
Support during menstrual migraines is less about forcing relief and more about reducing load.
Helpful principles include:
1. Reduce Sensory Input Before the Peak
During the days leading up to your migraine window, your brain benefits from fewer demands:
-
Softer lighting
-
Lower noise exposure
-
Fewer multitasking demands
Think of this as conserving sensory bandwidth.
2. Prioritise Nervous System Safety
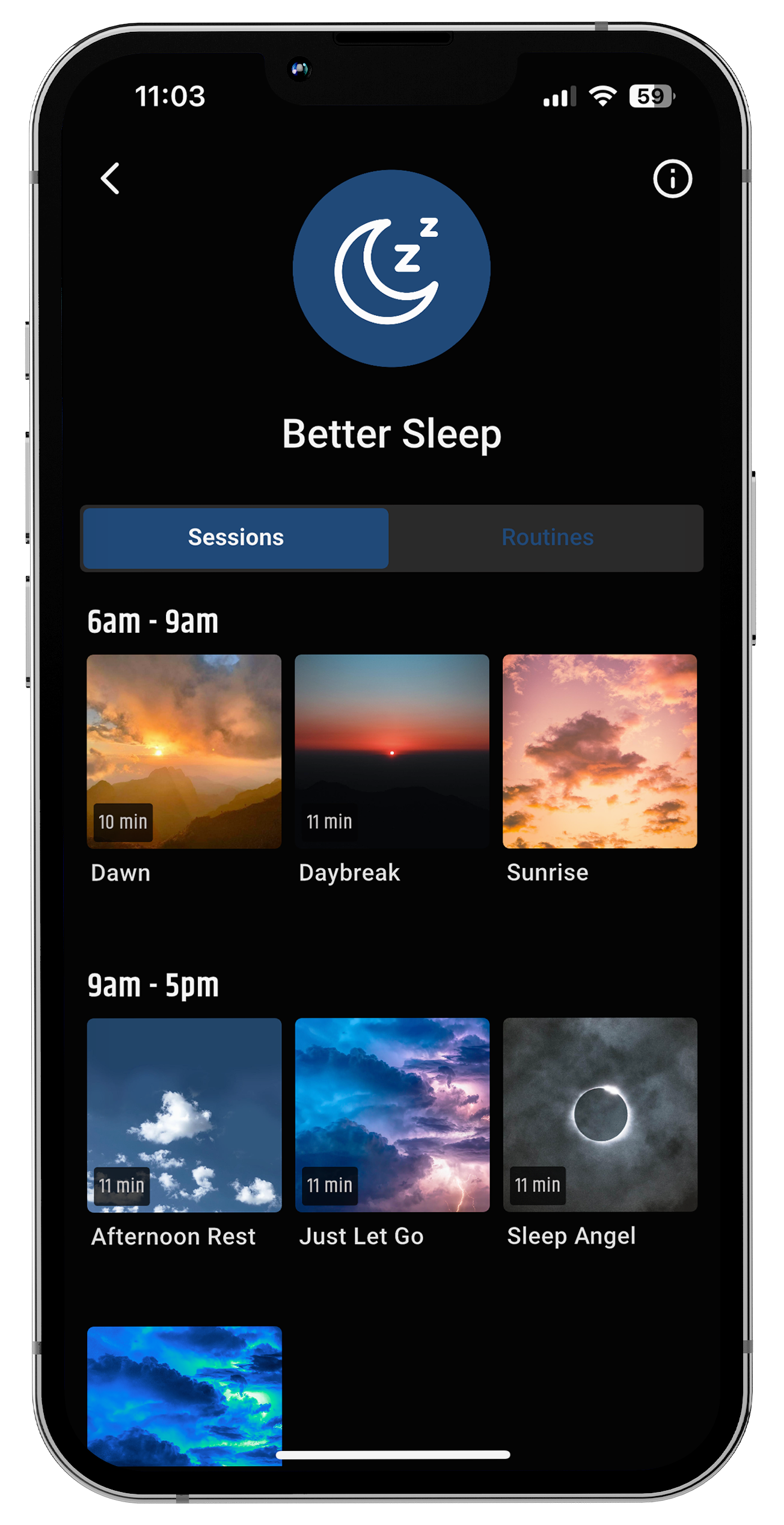
Predictability helps regulate a sensitive brain. Gentle routines, regular sleep timing, and calmer transitions signal safety to the nervous system.
This isn’t about strict rules, it's about creating a rhythm your brain can trust.
3. Use Gentle Sensory Support
Because the brain is already overloaded, support should be non-invasive and calming, not stimulating.
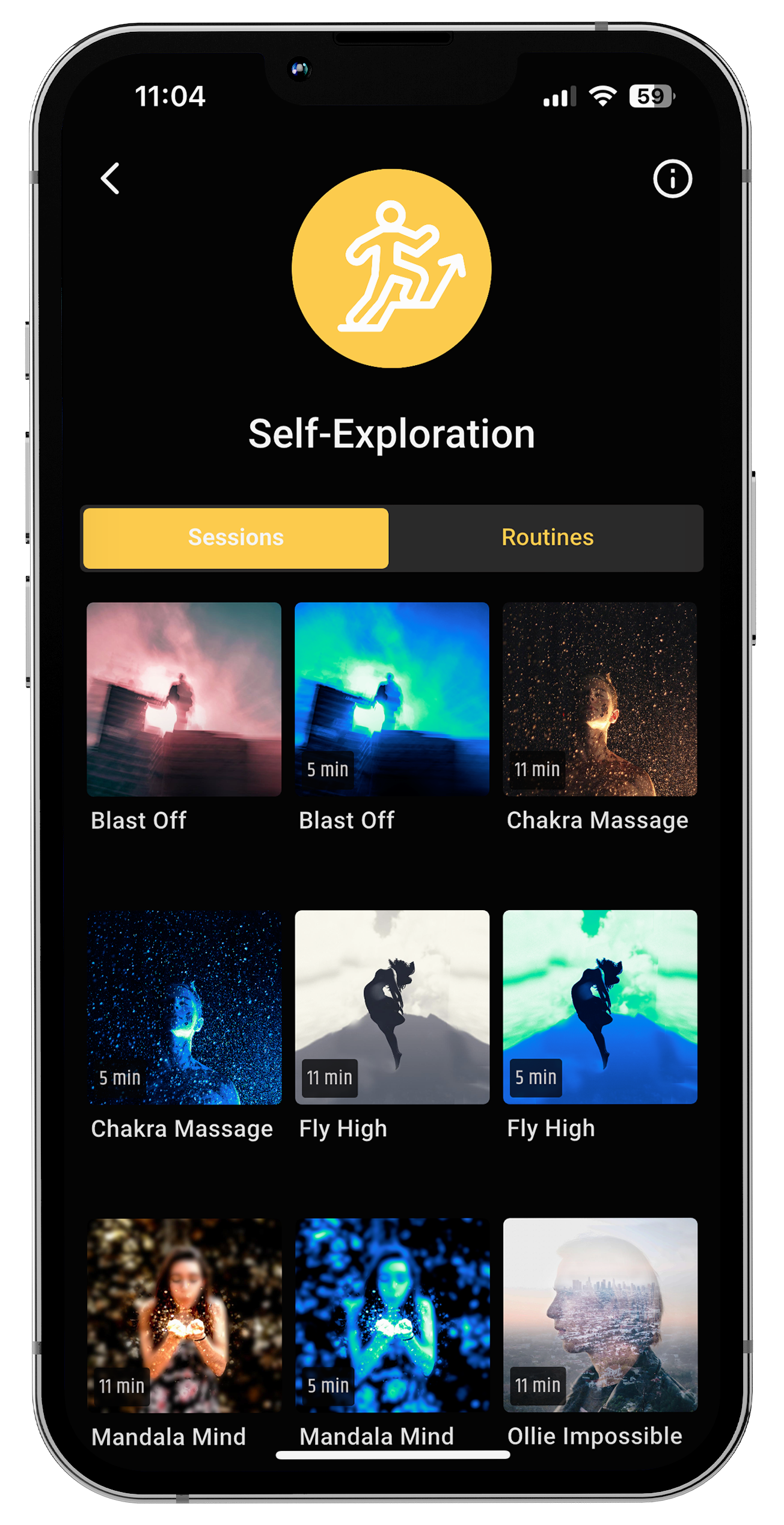
Some people find relief through controlled light and sound experiences designed to support regulation rather than overwhelm. When used gently, these inputs can help the brain settle instead of escalate.
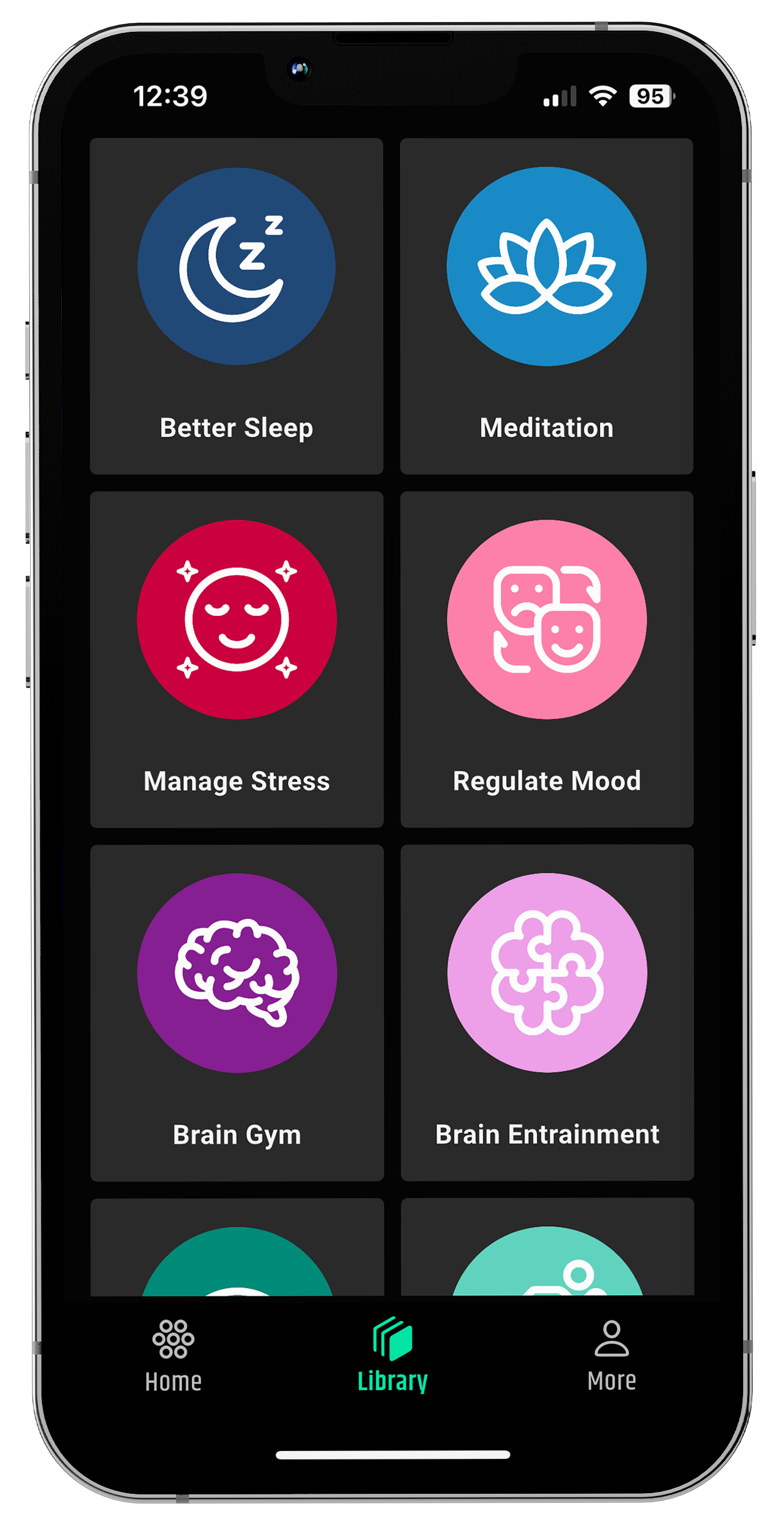
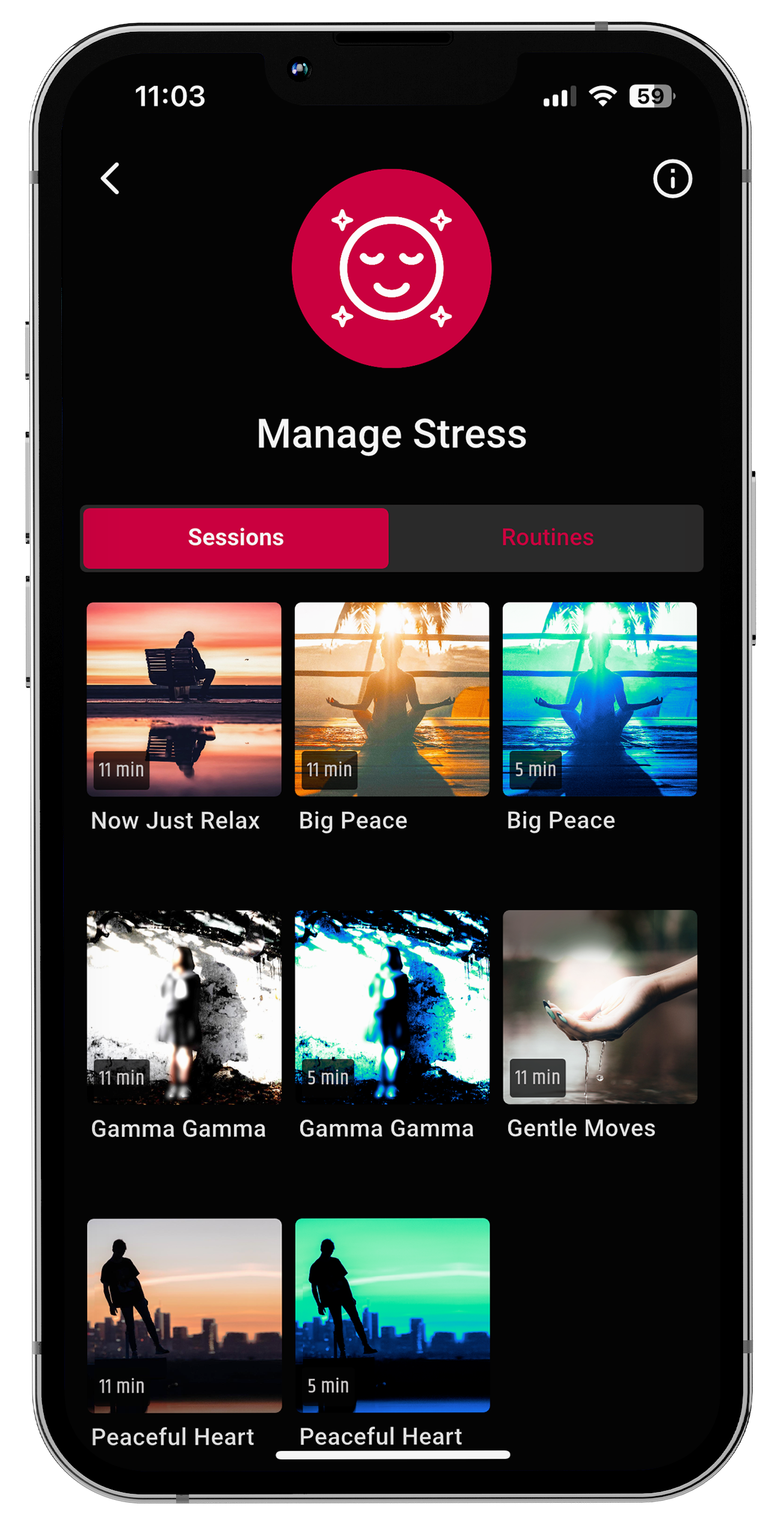
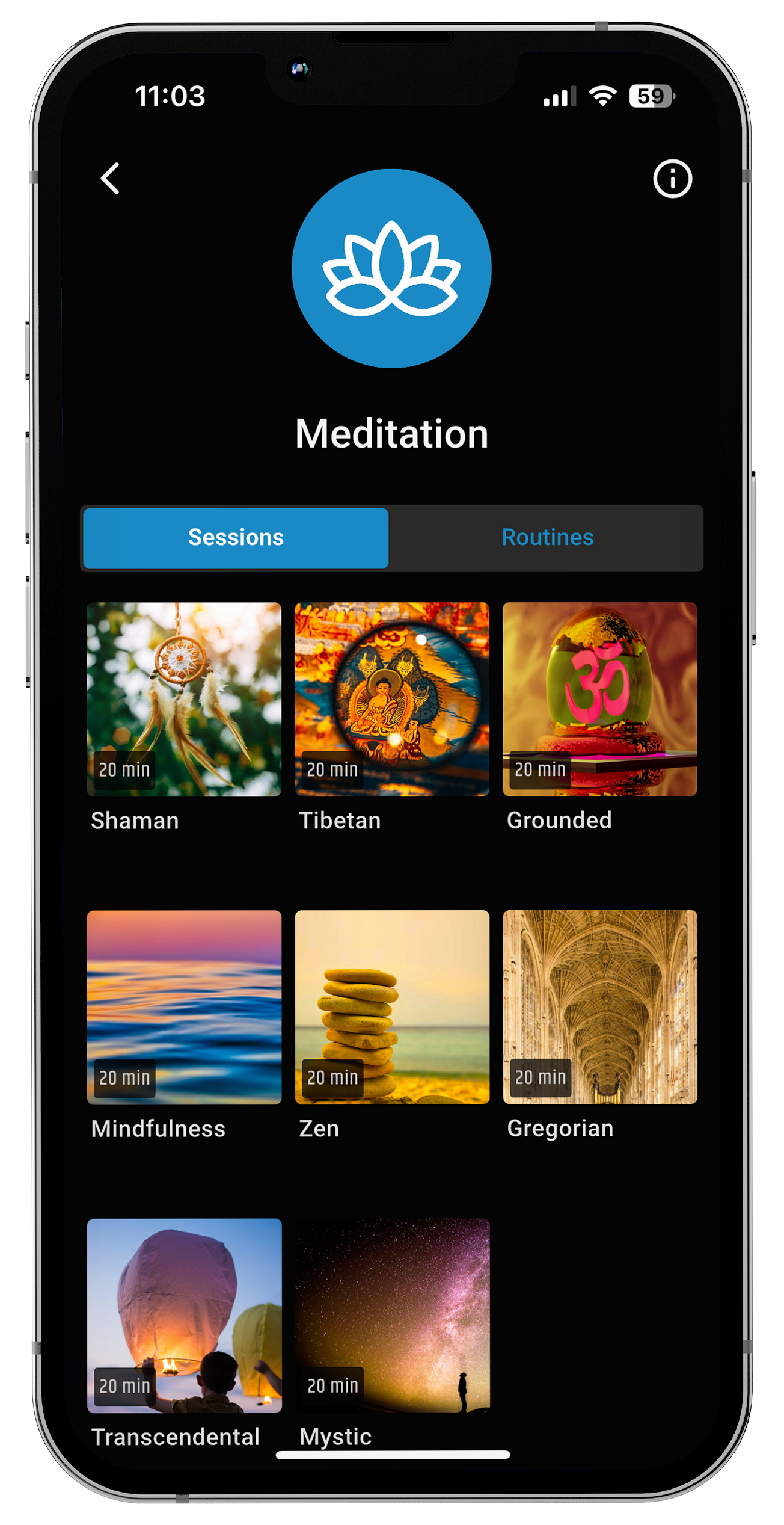
At neuroVIZR, the focus is on supporting brain states not pushing performance especially during sensitive phases like hormonal transitions.
How This Awareness Can Change Your Relationship With Migraines
Understanding menstrual migraines as a brain-state shift can soften the internal struggle.
Instead of asking:
“What’s wrong with me?”
The question becomes:
“What does my brain need right now?”
That shift alone reduces stress and stress is a powerful amplifier of migraine severity.
Many people find that when they stop fighting their nervous system and start listening to it, migraines feel less frightening, even if they still occur. Relief isn’t always immediate, but self-trust grows.
How neuroVIZR May Offer Support During Menstrual Migraines
Menstrual migraines often coincide with a period when the brain becomes more sensitive to light, sound, and internal signals. During this window, the goal isn’t to “push through” or stimulate the brain, it's to create conditions that feel calmer and more predictable.
neuroVIZR is designed as a light and sound neurotechnology experience that some people choose to use during moments of heightened sensitivity. Rather than targeting migraines directly, it focuses on supporting overall brain-state regulation.
A Grounded Takeaway
Menstrual migraines don’t mean your body is failing you.
They mean your brain is temporarily more sensitive and sensitivity isn't a weakness.
With awareness, gentler support, and nervous-system-first strategies, it’s possible to move through these phases with more understanding and less self-blame.
At neuroVIZR, we believe brain wellness begins with listening especially during the moments when your brain is asking for care, not control.
FAQs
Why do migraines happen around my period?
Migraines around menstruation happen because hormonal shifts, especially changes in estrogen, can affect how the brain processes pain, light, and sound, making the nervous system more reactive.
Why are menstrual migraines more intense than regular headaches?
Menstrual migraines often feel more intense because the brain’s ability to filter sensory input is reduced during this phase, which can amplify light sensitivity, sound intolerance, and pain perception.
Are menstrual migraines caused only by hormones?
Hormones play a role, but menstrual migraines also involve nervous system regulation, sensory processing, and how the brain responds to internal and external stimuli during hormonal transitions.
Can stress make menstrual migraines worse?
Stress can increase nervous system load, which may intensify menstrual migraines, especially when the brain is already in a more sensitive state during the menstrual cycle.
Content Reference
-
American Migraine Foundation
-
National Institute of Neurological Disorders and Stroke (NINDS)
-
International Headache Society
-
The Migraine Trust
-
Mayo Clinic
-
Cleveland Clinic
Disclaimer
This content is for informational purposes only and does not provide medical advice. neuroVIZR is not intended to diagnose, treat, cure, or prevent migraines or any health condition. Individual experiences may vary. Always consult a qualified healthcare professional for medical concerns.


















Share:
Perimenopause Anxiety Disorder: Causes, Symptoms, Diagnosis & Treatment
Can Perimenopause Cause Headaches?