You are not alone, if you have ever wondered whether this is a perimenopause headache or you are imagining it. During perimenopause, headache is quite normal, actual and based on the way your brain reacts to the changing hormones. And knowing the reason why can make you feel less rejected.
The perimenopause headaches are not accidental. They arise as a result of an intense interaction between hormones, neural sensitivity, and the brain pain-processing systems. And unlike tension or stress-headaches, they have a relation with biological rhythms varying within you. Let us not unpack too hard what we have to do.
Why Perimenopause May Cause Headaches
The first period is perimenopause, the period leading up to menopause, during which your hormonal system is booting up again particularly estrogen and progesterone. These hormones do not merely go down, they are insane and varying day in, day out, week in, week out. Estrogen can affect such neurotransmitters as serotonin and dopamine but this phenomenon is involved in the process of pain perception and blood-vessel behaviour regulation in the brain.
These fluctuations up and down of estrogen particularly those periods when it falls greatly out of control can cause a direct effect on the sensitivity of your brain to pains.
The peculiarity of this to perimenopause (as opposed to a typical tension headache) is the impact of these hormone changes on the blood-brain interaction and neural pain circuits. Estrogen bypasses the blood-brain barrier and helps to mediate the pain-processing chemicals in your central nervous system. In such a case when it becomes unpredictable, then your brain sends you a signal of instability and you may end up having headaches.
In the real world, it has the implication of what might have been a low frequency headache when you were younger, being more frequent, more severe, or of a different quality on perimenopause.
Different Types of Headaches During Perimenopause
1. Hormonal Migraines
If you’ve ever had migraines in relation to your menstrual cycle, perimenopause might worsen those episodes. Hormonal migraines are linked to estrogen fluctuations, especially the sudden drop known as “estrogen withdrawal.” These migraines often come with light sensitivity, nausea, or throbbing pain on one or both sides of the head.
This is similar to what many people report in our neuroVIZR community, where migraine sensitivity seems connected not just to stress but to underlying neural sensitivity that gets amplified by hormone swings much like what’s discussed in our Menstrual Migraines: When Your Brain Becomes More Sensitive article. That piece explores how certain brains are wired to respond more intensely to internal triggers, including hormones.
2. Tension-Type Headaches
These headaches feel like a tight band around your head. They are often related to stress, sleep disruption, or muscular tension around the neck and jaw all of which perimenopause can exacerbate through cortisol shifts and nervous system responses.
Triggers That Make Headaches Worse
Headaches in perimenopause don’t happen in isolation. There are everyday triggers that can amplify them:
-
Sleep disruption: Hot flashes and night sweats fragment sleep, which sensitises the brain to pain.
-
Stress and autonomic tension: Chronic stress increases cortisol, tightening muscles and lowering your pain threshold.
-
Hydration and diet: Changes in routine, dehydration, caffeine variations, or certain foods can tip your nervous system toward headache triggers.
-
Emotional load: Anxiety, mood swings, or worry which can be heightened during perimenopause also affect neural circuitry involved in pain regulation.
At its core, a perimenopausal headache isn’t just “a headache” it’s your central nervous system responding to many internal shifts at once.
How to Work With These Headaches
There’s no single quick fix but there is a path toward relief that honours both your brain’s biology and your lived experience:
1. Track Patterns
Notice when headaches happen: time of day, relation to sleep, stress, or meals. That gives your brain a narrative not just a pain that “comes out of nowhere.”
2. Nervous System Regulation
Simple practices like breathwork, grounding, and light touch self-soothing help calm the autonomic nervous system, which in turn lowers sensitivity to pain.
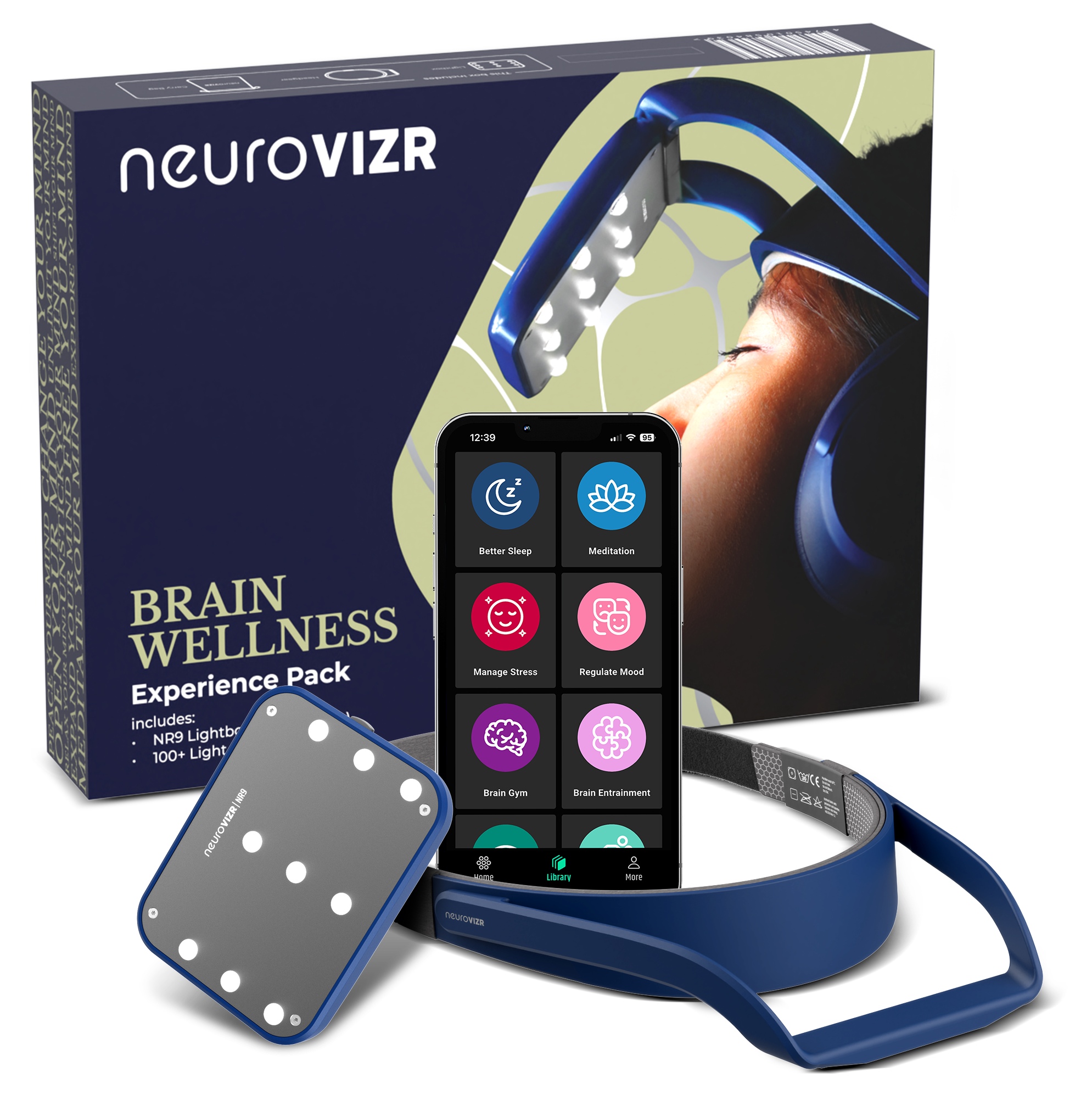
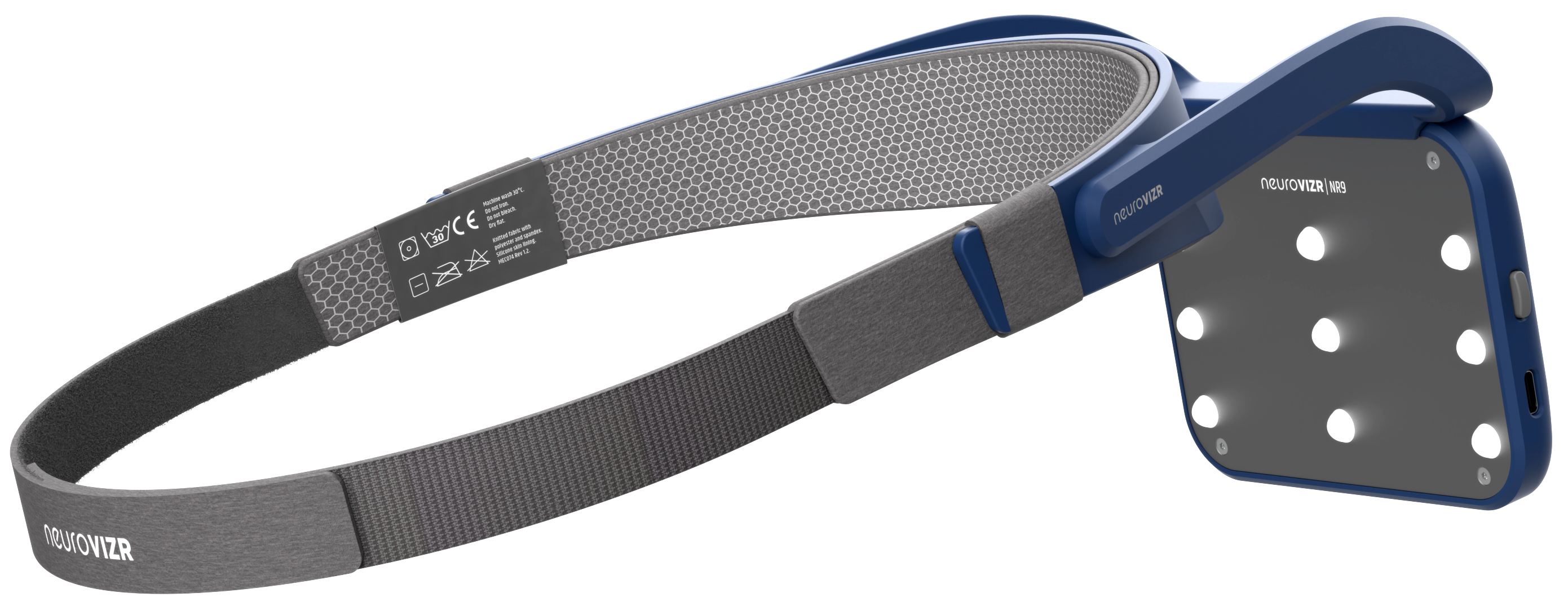
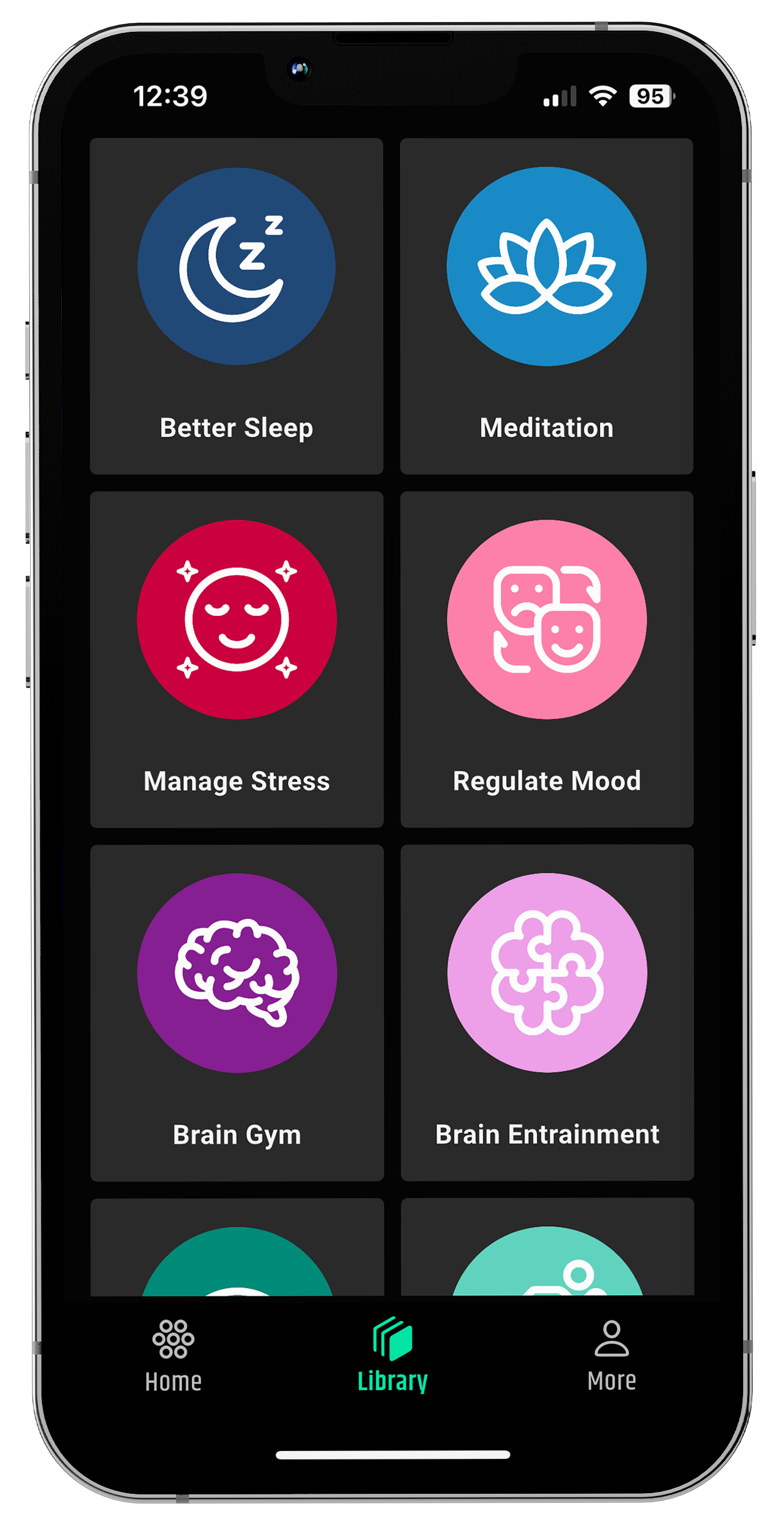
This is why many people find approaches that support brain regulation helpful. For example, technologies like neuroVIZR can assist with neural coherence and stress reduction, helping you quiet the nervous system without medication. The device’s light and sound patterns are designed to guide your brain into calmer states potentially offering relief when hormones make your brain feel oversensitive.
3. Consistent Sleep & Routine
Stabilising circadian rhythms helps buffer your nervous system against hormone-induced fluctuations.
4. Professional Support
If headaches are severe, change suddenly, or come with neurological symptoms (like vision changes or numbness), that’s a cue to talk with a healthcare provider.
Conclusion
The existence of perimenopause headaches is not a myth and they have a very complicated and dynamic interaction between your hormones and nervous system. That is the same way you can know that you are in agency rather than in confusion.
It is not your brain going bad, but getting used to change. By softly monitoring yourself, providing support to the nervous system, and maintaining regular routines, as well as being kind to yourself, you will be able to cope with such headaches without experiencing fear.
And should perimenopause also rouse anxiety or mood irritability, then you may find further background in our article on perimenopause anxiety disorder in which we discuss how the changing hormones influence both mood and the neural control.
FAQ’s
Can perimenopause cause headaches even if I never had them before?
Yes. Many people experience headaches for the first time during perimenopause due to fluctuating estrogen levels, changes in sleep, and increased nervous system sensitivity.
Are perimenopause headaches usually migraines or tension headaches?
They can be both. Some people develop hormonal migraines linked to estrogen drops, while others experience tension-type headaches related to stress, muscle tightness, or poor sleep.
Do perimenopause headaches happen at specific times?
Often, yes. Headaches may appear around irregular cycles, during high stress periods, after poor sleep, or in the morning when hormone and cortisol levels shift.
Can anxiety during perimenopause make headaches worse?
Yes. Anxiety activates the stress response, which can increase muscle tension and lower pain tolerance. Hormonal changes can heighten this brain–body sensitivity.
Content source
-
Mayo Clinic
-
Healthline
-
Vitalia Health
-
MLRB (Medical & Lifestyle Research Blog)
Disclaimer
This content is for informational and educational purposes only and is not intended as medical advice, diagnosis, or treatment. neuroVIZR does not replace professional healthcare guidance. Always consult a qualified healthcare provider regarding any medical condition, symptoms, or treatment decisions.

















Share:
Menstrual Migraines: When Your Brain Becomes More Sensitive
Understanding Anxiety in Perimenopause